Predicting human tissue exposures to xenobiotics using a bottom-up physiologically-based biokinetic model
Main Article Content
Abstract
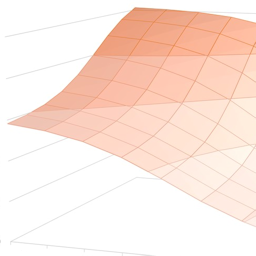
Advances in physiologically-based biokinetic (PBK) modelling, in vitro-to-in vivo extrapolation (IVIVE) methodologies, and development of permeability-limited biokinetic models have allowed predictions of tissue drug concentrations without utilizing in vivo animal or human data. However, there is a lack of in vivo human tissue concentrations to validate these models. Herein, we validated the performance of our previously published bottom-up rosuvastatin (RSV) PBK model with clinical data from a recently published study that made use of positron emission tomography (PET) imaging to quantify the hepatic concentrations of [11C]RSV drug-drug interaction (DDI) with cyclosporine A (CsA). Simulated RSV area under the plasma concentration-time curve (AUC0h-t) and maximum plasma concentration (Cmax) before and after DDI were within 1.5-fold of the observed data. Simulated AUC0-30min and Cmax ratios in the DDI setting matched the observed ratios closely (within 1.1-fold). To predict RSV hepatic concentrations, the model inputs were modified to account for RSV in the bile canaliculi after biliary excretion. The model recapitulated the observed hepatic concentrations before DDI and the decrease in hepatic concentrations after DDI. Simulated area under the liver concentration-time curve (AUC0-30min,liver), maximum liver concentration (Cmax,liver), AUC0-30min,liver ratio and Cmax,liver ratios were predicted within 1.5-fold of the observed data. In summary, we validated the ability of bottom-up PBK modelling to predict RSV hepatic concentrations with and without DDI with CsA. Our findings confirm the importance to account for drug distributed within the bile canaliculi for accurate prediction of hepatic tissue drug levels when compared against in vivo liver PET scan data.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Articles are distributed under the terms of the Creative Commons Attribution 4.0 International license (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is appropriately cited (CC-BY). Copyright on any article in ALTEX is retained by the author(s).
Astra Zeneca (2003). Product Information Leaflet: Crestor, Rosuvastatin Calcium Tablets.
Benet, L. Z., Broccatelli, F. and Oprea, T. I. (2011). BDDCS applied to over 900 drugs. AAPS J 13, 519-547. doi:10.1208/s12248-011-9290-9
Bi, Y., Qiu, X., Rotter, C. J. et al. (2013). Quantitative assessment of the contribution of sodium-dependent taurocholate co-transporting polypeptide (NTCP) to the hepatic uptake of rosuvastatin, pitavastatin and fluvastatin. Biopharm Drug Dispos 34, 452-461. doi:10.1002/bdd.1861
Billington, S., Shoner, S., Lee, S. et al. (2019). Positron emission tomography imaging of [11C]rosuvastatin hepatic concentrations and hepatobiliary transport in humans in the absence and presence of cyclosporin A. Clin Pharmacol Ther 106, 1056-1066. doi:10.1002/cpt.1506
Bosgra, S., Van De Steeg, E., Vlaming, M. L. et al. (2014). Predicting carrier-mediated hepatic disposition of rosuvastatin in man by scaling from individual transfected cell-lines in vitro using absolute transporter protein quantification and PBPK modeling. Eur J Pharm Sci 65, 156-166. doi:10.1016/j.ejps.2014.09.007
Boyer, J. L. (2013). Bile Formation and Secretion. In Comprehensive Physiology (1035-1078). Hoboken, NJ, USA: John Wiley & Sons, Inc. doi:10.1002/cphy.c120027
Chan, J. C. Y., Tan, S. P. F., Upton, Z. et al. (2019). Bottom-up physiologically-based biokinetic modelling as an alternative to animal testing. ALTEX 36, 597-612. doi:10.14573/altex.1812051
Chu, X., Korzekwa, K., Elsby, R. et al. (2013). Intracellular drug concentrations and transporters: Measurement, modeling, and implications for the liver. Clin Pharmacol Ther 94, 126-141. doi:10.1038/clpt.2013.78
Fujino, H., Saito, T., Tsunenari, Y. et al. (2004). Metabolic properties of the acid and lactone forms of HMG-CoA reductase inhibitors. Xenobiotica 34, 961-971. doi:10.1080/00498250400015319
Guo, Y., Chu, X., Parrott, N. J. et al. (2018). Advancing predictions of tissue and intracellular drug concentrations using in vitro, imaging and physiologically based pharmacokinetic modeling approaches. Clin Pharmacol Ther 104, 865-889. doi:10.1002/cpt.1183
Huang, W. and Isoherranen, N. (2018). Development of a dynamic physiologically based mechanistic kidney model to predict renal clearance. CPT Pharmacometrics Syst Pharmacol 7, 593-602. doi:10.1002/psp4.12321
Izumi, S., Nozaki, Y., Kusuhara, H. et al. (2018). Relative activity factor (RAF)-based scaling of uptake clearance mediated by organic anion transporting polypeptide (OATP) 1B1 and OATP1B3 in human hepatocytes. Mol Pharm 15, 2277-2288. doi:10.1021/acs.molpharmaceut.8b00138
Jamei, M., Bajot, F., Neuhoff, S. et al. (2014). A mechanistic framework for in vitro-in vivo extrapolation of liver membrane transporters: Prediction of drug-drug interaction between rosuvastatin and cyclosporine. Clin Pharmacokinet 53, 73-87. doi:10.1007/s40262-013-0097-y
Jones, H. M., Barton, H. A., Lai, Y. et al. (2012). Mechanistic pharmacokinetic modelling for the prediction of transporter-mediated disposition in human from sandwich culture human hepatocyte data. Drug Metab Dispos 40, 1007-1017. doi:10.1124/dmd.111.042994
Kaneko, K.-I., Tanaka, M., Ishii, A. et al. (2018). A clinical quantitative evaluation of hepatobiliary transport of [11C] dehydropravastatin in humans using positron emission tomography. Drug Metab Dispos 46, 719-728. doi:10.1124/dmd.118.080408
Li, J., Volpe, D. A., Wang, Y. et al. (2011). Use of transporter knockdown Caco-2 cells to investigate the in vitro efflux of statin drugs. Drug Metab Dispos 39, 1196-1202. doi:10.1124/dmd.111.038075
Loreno, M., Travali, S., Bucceri, A. M. et al. (2009). Ultrasonographic study of gallbladder wall thickness and emptying in cirrhotic patients without gallstones. Gastroenterol Res Pract 2009, 683040. doi:10.1155/2009/683040
Martin, P. D., Mitchell, P. D. and Schneck, D. W. (2002). Pharmacodynamic effects and pharmacokinetics of a new HMG-CoA reductase inhibitor, rosuvastatin, after morning or evening administration in healthy volunteers. Br J Clin Pharmacol 54, 472-477. doi:10.1046/j.1365-2125.2002.01688.x
Martin, P. D., Warwick, M. J., Dane, A. L. et al. (2003). Absolute oral bioavailability of rosuvastatin in healthy white adult male volunteers. Clin Ther 25, 2553-2563. doi:10.1016/S0149-2918(03)80316-8
McTaggart, F., Buckett, L., Davidson, R. et al. (2001). Preclinical and clinical pharmacology of rosuvastatin, a new 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitor. Am J Cardiol 87, 28-32. doi:10.1016/S0002-9149(01)01454-0
Paini, A., Leonard, J. A., Joossens, E. et al. (2019). Next generation physiologically based kinetic (NG-PBK) models in support of regulatory decision making. Comput Toxicol 9, 61-72. doi:10.1016/j.comtox.2018.11.002
Pfeifer, N. D., Yang, K. and Brouwer, K. L. R. (2013). Hepatic basolateral efflux contributes significantly to rosuvastatin disposition I: Characterization of basolateral versus biliary clearance using a novel protocol in sandwich-cultured hepatocytes. J Pharmacol Exp Ther 347, 727-736. doi:10.1124/jpet.113.207472
Punt, A., Peijnenburg, A. A. C. M., Hoogenboom, R. L. A. P. et al. (2017). Non-animal approaches for toxicokinetics in risk evaluations of food chemicals. ALTEX 34, 501-514. doi:10.14573/altex.1702211
Riccardi, K., Lin, J., Li, Z. et al. (2017). Novel method to predict in vivo liver-to-plasma Kpuu for OATP substrates using suspension hepatocytes. Drug Metab Dispos 45, 576-580. doi:10.1124/dmd.116.074575
Rodgers, T., Leahy, D. and Rowland, M. (2005). Physiologically based pharmacokinetic modeling 1: Predicting the tissue distribution of moderate-to-strong bases. J Pharm Sci 94, 1259-1276. doi:10.1002/jps.20322
Rodgers, T. and Rowland, M. (2006). Physiologically based pharmacokinetic modelling 2: Predicting the tissue distribution of acids, very weak bases, neutrals and zwitterions. J Pharm Sci 95, 1238-1257. doi:10.1002/jps.20502
Rodgers, T. and Rowland, M. (2007). Mechanistic approaches to volume of distribution predictions: Understanding the processes. Pharm Res 24, 918-933. doi:10.1007/s11095-006-9210-3
Ryu, S., Tess, D., Chang, G. et al. (2020). Evaluation of fraction unbound across 7 tissues of 5 species. J Pharm Sci 109, 1178-1190. doi:10.1016/j.xphs.2019.10.060
Schirris, T. J. J., Ritschel, T., Bilos, A. et al. (2015). Statin lactonization by uridine 5′-diphospho-glucuronosyltransferases (UGTs). Mol Pharm 12, 4048-4055. doi:10.1021/acs.molpharmaceut.5b00474
Simonson, S. G., Raza, A., Martin, P. D. et al. (2004). Rosuvastatin pharmacokinetics in heart transplant recipients administered an antirejection regimen including cyclosporine. Clin Pharmacol Ther 76, 167-177. doi:10.1016/j.clpt.2004.03.010
Steffansen, B., Nielsen, C. U. and Brodin, B. (2015). Membrane Transporters in ADME. In Y. Sugiyama and B. Steffansen (eds.), Transporters in Drug Development: Discovery, Optimization, Clinical Study and Regulation (1-22). AAPS Advances in the Pharmaceutical Sciences Series, Volume 7. New York, NY, USA: Springer. doi:10.1007/978-1-4614-8229-1
Sun, D., Lennernas, H., Welage, L. S. et al. (2002). Comparison of human duodenum and Caco-2 gene expression profiles for 12,000 gene sequences tags and correlation with permeability of 26 drugs. Pharm Res 19, 1400-1416. doi:10.1023/A:1020483911355
US Food and Drug Adminstration (2020). Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers. https://www.fda.gov/drugs/drug-interactions-labeling/drug-development-and-drug-interactions-table-substrates-inhibitors-and-inducers#table5-1 (accessed 17.03.2020)
Verhulst, A., Sayer, R., De Broe, M. E. et al. (2008). Human proximal tubular epithelium actively secretes but does not retain rosuvastatin. Mol Pharmacol 74, 1084-1091. doi:10.1124/mol.108.047647
Vildhede, A., Karlgren, M., Svedberg, E. K. et al. (2014). Hepatic uptake of atorvastatin: Influence of variability in transporter expression on uptake clearance and drug-drug interactions. Drug Metab Dispos 42, 1210-1218. doi:10.1124/dmd.113.056309
Wang, Q., Zheng, M. and Leil, T. (2017). Investigating transporter-mediated drug-drug interactions using a physiologically based pharmacokinetic model of rosuvastatin. CPT Pharmacometrics Syst Pharmacol 6, 228-238. doi:10.1002/psp4.12168
Yoshikado, T., Toshimoto, K., Nakada, T. et al. (2017). Comparison of methods for estimating unbound intracellular-to-medium concentration ratios in rat and human hepatocytes using statins. Drug Metab Dispos 45, 779-789. doi:10.1124/dmd.116.074823
Zhang, D., Donohue, A. F., Dragovich, P. S. et al. (2019a). Special section on pharmacokinetic and drug metabolism properties of novel therapeutic modalities catalytic cleavage of disulfide bonds in small molecules and linkers of antibody – Drug conjugates. Drug Metab Dispos 47, 1156-1163. doi:10.1124/dmd.118.086132
Zhang, D., Hop, C. E. C. A., Patilea-Vrana, G. et al. (2019b). Drug concentration asymmetry in tissues and plasma for small molecule-related therapeutic modalities. Drug Metab Dispos 47, 1122-1135. doi:10.1124/dmd.119.086744