The future of Parkinson’s disease research: A new paradigm of human specific investigation is necessary… and possible
Main Article Content
Abstract
Parkinson’s disease (PD) is a complex neurodegenerative condition with a multifactorial origin. To date, approaches to drug discovery for PD have resulted in symptomatic therapies for the motor manifestations and signs associated with neurodegeneration but have failed to identify preventive or curative therapies. This failure mainly originates from the persistence of major gaps in our understanding of the specific molecular basis of PD initiation and progression. New approach methodologies (NAMs) hold the potential to advance PD research while facilitating a move away from animal- based research. We report a workshop involving NAM experts in the field of PD and neurodegenerative diseases, who discussed and identified a scientific strategy for successful, human-specific PD research. We outline some of the most important human-specific NAMs, along with their main potentials and limitations, and suggest possible ways to overcome the latter. Key recommendations to advance PD research include integrating NAMs while accounting for multiple levels of complexity, from molecular to population level; learning from recent advances in Alzheimer’s disease research; increasing the sharing of data; promoting innovative pilot studies on disease pathogenesis; and accessing philanthropic funding to enable studies using novel approaches. Collaborative efforts between different stakeholders, including researchers, clinicians, and funding agencies, are urgently needed to create a scientific roadmap and support a paradigm change towards effective, human-specific research for neurodegenerative diseases without animals, as is already happening in the field of toxicology.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Articles are distributed under the terms of the Creative Commons Attribution 4.0 International license (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is appropriately cited (CC-BY). Copyright on any article in ALTEX is retained by the author(s).
Abd Elhadi, S., Grigoletto, J., Poli, M. et al. (2019). α-synuclein in blood cells differentiates Parkinson’s disease from healthy controls. Ann Clin Transl Neurol 6, 2426-2436. doi:10.1002/acn3.50944
Abounit, S., Bousset, L., Loria, F. et al. (2016). Tunneling nanotubes spread fibrillar α-synuclein by intercellular trafficking of lysosomes. Embo J 35, 2120-2138. doi:10.15252/embj.201593411
Adams, B., Nunes, J. M., Page, M. J. et al. (2019). Parkinson’s disease: A systemic inflammatory disease accompanied by bacterial inflammagens. Front Aging Neurosci 11, 210. doi:10.3389/fnagi.2019.00210
Agrawal, M. and Biswas, A. (2015). Molecular diagnostics of neurodegenerative disorders. Front Mol Biosci 2, 54. doi:10.3389/fmolb.2015.00054
Baggio, H. C. and Junqué, C. (2019). Functional MRI in Parkinson’s disease cognitive impairment. Int Rev Neurobiol 144, 29-58. doi:10.1016/bs.irn.2018.09.010
Bailey, J. and Balls, M. (2019). Recent efforts to elucidate the scientific validity of animal-based drug tests by the pharmaceutical industry, pro-testing lobby groups, and animal welfare organisations. BMC Med Ethics 20, 16. doi:10.1186/s12910-019-0352-3
Balestrino, R. and Schapira, A. H. V. (2020). Parkinson disease. Eur J Neurol 27, 27-42. doi:10.1111/ene.14108
Ball, N., Teo, W. P., Chandra, S. et al. (2019). Parkinson’s disease and the environment. Front Neurol 10, 218. doi:10.3389/fneur.2019.00218
Bhatia, S. N. and Ingber, D. E. (2014). Microfluidic organs-on-chips. Nat Biotechnol 32, 760-772. doi:10.1038/nbt.2989
Blauwendraat, C., Heilbron, K., Vallerga, C. L. et al. (2019). Parkinson’s disease age at onset genome-wide association study: Defining heritability, genetic loci, and α-synuclein mechanisms. Mov Disord 34, 866-875. doi:10.1002/mds.27659
Borghammer, P. and Van Den Berge, N. (2019). Brain-first versus gut-first Parkinson’s disease: A hypothesis. J Parkinsons Dis 9, S281-S295. doi:10.3233/JPD-191721
Borrageiro, G., Haylett, W., Seedat, S. et al. (2018). A review of genome-wide transcriptomics studies in Parkinson’s disease. Eur J Neurosci 47, 1-16. doi:10.1111/ejn.13760
Brás, I. C., Dominguez-Meijide, A., Gerhardt, E. et al. (2020). Synucleinopathies: Where we are and where we need to go. J Neurochem 153, 433-454. doi:10.1111/jnc.14965
Buchman, A. S., Yu, L., Wilson, R. S. et al. (2019). Progressive parkinsonism in older adults is related to the burden of mixed brain pathologies. Neurology 92, e1821-e1830. doi:10.1212/wnl.0000000000007315
Carney, E. F. (2020). Pharmacokinetic modelling using linked organ chips. Nat Rev Nephrol 16, 188. doi:10.1038/s41581-020-0257-x
Cavanaugh, S. E., Pippin, J. J. and Barnard, N. D. (2014). Animal models of Alzheimer disease: Historical pitfalls and a path forward. ALTEX 31, 279-302. doi:10.14573/altex.1310071
Day, J. O. and Mullin, S. (2021). The genetics of Parkinson’s disease and implications for clinical practice. Genes (Basel) 12, 1006. doi:10.3390/genes12071006
De Micco, R., Agosta, F., Basaia, S. et al. (2021). Functional connectomics and disease progression in drug-naïve Parkinson’s disease patients. Mov Disord 36, 1603-1616. doi:10.1002/mds.28541
Dixit, A., Mehta, R. and Singh, A. K. (2019). Proteomics in human Parkinson’s disease: Present scenario and future directions. Cell Mol Neurobiol 39, 901-915. doi:10.1007/s10571-019-00700-9
Dong, M. X., Feng, X., Xu, X. M. et al. (2018). Integrated analysis reveals altered lipid and glucose metabolism and identifies NOTCH2 as a biomarker for Parkinson’s disease related depression. Front Mol Neurosci 11, 257. doi:10.3389/fnmol.2018.00257
Efremova, L., Schildknecht, S., Adam, M. et al. (2015). Prevention of the degeneration of human dopaminergic neurons in an astrocyte co-culture system allowing endogenous drug metabolism. Br J Pharmacol 172, 4119-4132. doi:10.1111/bph.13193
Falkenburger, B. H., Saridaki, T. and Dinter, E. (2016). Cellular models for Parkinson’s disease. J Neurochem 139, Suppl 1, 121-130. doi:10.1111/jnc.13618
Fernandes, H. J. R., Patikas, N., Foskolou, S. et al. (2020). Single-cell transcriptomics of Parkinson’s disease human in vitro models reveals dopamine neuron-specific stress responses. Cell Rep 33, 108263. doi:10.1016/j.celrep.2020.108263
Ferrari, E., Palma, C., Vesentini, S. et al. (2020). Integrating biosensors in organs-on-chip devices: A perspective on current strategies to monitor microphysiological systems. Biosensors (Basel) 10, 110. doi:10.3390/bios10090110
Foo, J. N., Chew, E. G. Y., Chung, S. J. et al. (2020). Identification of risk loci for Parkinson disease in Asians and comparison of risk between Asians and Europeans: A genome-wide association study. JAMA Neurol 77, 746-754. doi:10.1001/jamaneurol.2020.0428
Gaig, C. and Tolosa, E. (2009). When does Parkinson’s disease begin? Mov Disord 24, Suppl 2, S656-664. doi:10.1002/mds.22672
Geerts, H. (2009). Of mice and men: Bridging the translational disconnect in CNS drug discovery. CNS Drugs 23, 915-926. doi:10.2165/11310890-000000000-00000
Geerts, H., Spiros, A., Roberts, P. et al. (2013). Quantitative systems pharmacology as an extension of PK/PD modeling in CNS research and development. J Pharmacokinet Pharmacodyn 40, 257-265. doi:10.1007/s10928-013-9297-1
Geerts, H., Wikswo, J., van der Graaf, P. H. et al. (2020). Quantitative systems pharmacology for neuroscience drug discovery and development: Current status, opportunities, and challenges. CPT Pharmacometrics Syst Pharmacol 9, 5-20. doi:10.1002/psp4.12478
Gerding, H. R., Karreman, C., Daiber, A. et al. (2019). Reductive modification of genetically encoded 3-nitrotyrosine sites in alpha synuclein expressed in E.coli. Redox Biol 26, 101251. doi:10.1016/j.redox.2019.101251
Goldman, J. G., Andrews, H., Amara, A. et al. (2018). Cerebrospinal fluid, plasma, and saliva in the biofind study: Relationships among biomarkers and Parkinson’s disease features. Mov Disord 33, 282-288. doi:10.1002/mds.27232
Grenn, F. P., Kim, J. J., Makarious, M. B. et al. (2020). The Parkinson’s disease genome-wide association study locus browser. Mov Disord 35, 2056-2067. doi:10.1002/mds.28197
Grow, D. A., McCarrey, J. R. and Navara, C. S. (2016). Advantages of nonhuman primates as preclinical models for evaluating stem cell-based therapies for Parkinson’s disease. Stem Cell Res 17, 352-366. doi:10.1016/j.scr.2016.08.013
Harischandra, D. S., Rokad, D., Ghaisas, S. et al. (2020). Enhanced differentiation of human dopaminergic neuronal cell model for preclinical translational research in Parkinson’s disease. Biochim Biophys Acta Mol Basis Dis 1866, 165533. doi:10.1016/j.bbadis.2019.165533
Hartung, T. (2013). Look back in anger – What clinical studies tell us about preclinical work. ALTEX 30, 275-291. doi:10.14573/altex.2013.3.275
Hu, J. L., Todhunter, M. E., LaBarge, M. A. et al. (2018). Opportunities for organoids as new models of aging. J Cell Biol 217, 39-50. doi:10.1083/jcb.201709054
Ingber, D. E. (2020). Is it time for reviewer 3 to request human organ chip experiments instead of animal validation studies? Adv Sci (Weih) 7, 2002030. doi:10.1002/advs.202002030
Iwaki, H., Blauwendraat, C., Leonard, H. L. et al. (2019). Genomewide association study of Parkinson’s disease clinical biomarkers in 12 longitudinal patients’ cohorts. Mov Disord 34, 1839-1850. doi:10.1002/mds.27845
Jo, J., Xiao, Y., Sun, A. X. et al. (2016). Midbrain-like organoids from human pluripotent stem cells contain functional dopaminergic and neuromelanin-producing neurons. Cell Stem Cell 19, 248-257. doi:10.1016/j.stem.2016.07.005
Jo, J., Yang, L., Tran, H.-D. et al. (2021). Lewy body-like inclusions in human midbrain organoids carrying glucocerebrosidase and α-synuclein mutations. Ann Neurol 90, 490-505. doi:10.1002/ana.26166
Kano, M., Takanashi, M., Oyama, G. et al. (2020). Reduced astrocytic reactivity in human brains and midbrain organoids with prkn mutations. NPJ Parkinsons Dis 6, 33. doi:10.1038/s41531-020-00137-8
Kasendra, M., Tovaglieri, A., Sontheimer-Phelps, A. et al. (2018). Development of a primary human small intestine-on-a-chip using biopsy-derived organoids. Sci Rep 8, 2871. doi:10.1038/s41598-018-21201-7
Keshavarzian, A., Engen, P., Bonvegna, S. et al. (2020). The gut microbiome in Parkinson’s disease: A culprit or a bystander? Prog Brain Res 252, 357-450. doi:10.1016/bs.pbr.2020.01.004
Kim, H., Park, H. J., Choi, H. et al. (2019). Modeling G2019S-LRRK2 sporadic Parkinson’s disease in 3D midbrain organoids. Stem Cell Reports 12, 518-531. doi:10.1016/j.stemcr.2019.01.020
Kim, M.-H., Kim, D. and Sung, J. H. (2021). A gut-brain axis-on-a-chip for studying transport across epithelial and endothelial barriers. J Ind Eng Chem 101, 126-134. doi:10.1016/j.jiec.2021.06.021
King, A. (2018). The search for better animal models of Alzheimer’s disease. Nature 559, S13-S15. doi:10.1038/d41586-018-05722-9
Konnova, E. A. and Swanberg, M. (2018). Animal models of Parkinson’s disease. In T. B. Stoker and J. C. Greenland (eds.), Parkinson’s disease: Pathogenesis and clinical aspects (Chapter 5). Codon Publications. doi:10.15586/codonpublications.parkinsonsdisease.2018.ch5
Korat, Š., Bidesi, N. S. R., Bonanno, F. et al. (2021). Alpha-synuclein pet tracer development – An overview about current efforts. Pharmaceuticals 14, 847. doi:10.3390/ph14090847
Krassowski, M., Das, V., Sahu, S. K. et al. (2020). State of the field in multi-omics research: From computational needs to data mining and sharing. Front Genet 11, 610798. doi:10.3389/fgene.2020.610798
Krismer, F. and Seppi, K. (2021). The Parkinson disease connectome – Insights from new imaging studies. Nat Rev Neurol 17, 527-528. doi:10.1038/s41582-021-00543-3
Kwak, T. H., Kang, J. H., Hali, S. et al. (2020). Generation of homogeneous midbrain organoids with in vivo-like cellular composition facilitates neurotoxin-based Parkinson’s disease modeling. Stem Cells 38, 727-740. doi:10.1002/stem.3163
La Cognata, V., Morello, G. and Cavallaro, S. (2021). Omics data and their integrative analysis to support stratified medicine in neurodegenerative diseases. Int J Mol Sci 22, 4820.
Lebouvier, T., Chaumette, T., Paillusson, S. et al. (2009). The second brain and Parkinson’s disease. Eur J Neurosci 30, 735-741. doi:10.1111/j.1460-9568.2009.06873.x
Leist, M. and Hartung, T. (2013). Inflammatory findings on species extrapolations: Humans are definitely no 70-kg mice. Arch Toxicol 87, 563-567. doi:10.1007/s00204-013-1038-0
Liang, Y. and Yoon, J.-Y. (2021). In situ sensors for blood-brain barrier (BBB) on a chip. Sensor Actuator Rep 3, 100031. doi:10.1016/j.snr.2021.100031
Loane, C. and Politis, M. (2011). Positron emission tomography neuroimaging in Parkinson’s disease. Am J Transl Res 3, 323-341.
Loser, D., Hinojosa, M. G., Blum, J. et al. (2021). Functional alterations by a subgroup of neonicotinoid pesticides in human dopaminergic neurons. Arch Toxicol 95, 2081-2107. doi:10.1007/s00204-021-03031-1
Ma, J., Gao, J., Wang, J. et al. (2019). Prion-like mechanisms in Parkinson’s disease. Front Neurosci 13, 552. doi:10.3389/fnins.2019.00552
Mao, L., Zhang, Y., Tian, J. et al. (2021). Cross-sectional study on the gut microbiome of Parkinson’s disease patients in central china. Front Microbiol 12, 728479. doi:10.3389/fmicb.2021.728479
Marek, K., Jennings, D., Lasch S. et al. (2011). The Parkinson progression marker initiative (PPMI). Prog Neurobiol 95, 629-635. doi:10.1016/j.pneurobio.2011.09.005
Marshall, L. J. and Willett, C. (2018a). Parkinson’s disease research: Adopting a more human perspective to accelerate advances. Drug Discov Today 23, 1950-1961. doi:10.1016/j.drudis.2018.09.010
Marshall, L. J. and Willett, C. (2018b). Parkinson’s disease research: Adopting a more human perspective to accelerate advances. Drug Discov Today 23, 1950-1961. doi:10.1016/j.drudis.2018.09.010
Masato, A., Plotegher, N., Boassa, D. et al. (2019). Impaired dopamine metabolism in Parkinson’s disease pathogenesis. Mol Neurodegener 14, 35. doi:10.1186/s13024-019-0332-6
Mazuel, L., Chassain, C., Jean, B. et al. (2016). Proton MR spectroscopy for diagnosis and evaluation of treatment efficacy in Parkinson disease. Radiology 278, 505-513. doi:10.1148/radiol.2015142764
Mena, M. A., Casarejos, M. J., Solano, R. M. et al. (2009). Half a century of L-DOPA. Curr Top Med Chem 9, 880-893.
Mertens, J., Paquola, A. C. M., Ku, M. et al. (2015). Directly reprogrammed human neurons retain aging-associated transcriptomic signatures and reveal age-related nucleocytoplasmic defects. Cell Stem Cell 17, 705-718. doi:10.1016/j.stem.2015.09.001
Miller, J. D., Ganat, Y. M., Kishinevsky, S. et al. (2013). Human iPSC-based modeling of late-onset disease via progerin-induced aging. Cell Stem Cell 13, 691-705. doi:10.1016/j.stem.2013.11.006
Mizuno, Y., Shimoda, S. and Origasa, H. (2018). Long-term treatment of Parkinson’s disease with levodopa and other adjunctive drugs. J Neural Transm (Vienna) 125, 35-43. doi:10.1007/s00702-016-1671-x
Mohamed, N.-V., Sirois, J., Ramamurthy, J. et al. (2021). Midbrain organoids with an SNCA gene triplication model key features of synucleinopathy. Brain Commun 3, fcab223. doi:10.1093/braincomms/fcab223
Monzel, A. S., Hemmer, K., Kaoma, T. et al. (2020). Machine learning-assisted neurotoxicity prediction in human midbrain organoids. Parkinsonism Relat Disord 75, 105-109. doi:10.1016/j.parkreldis.2020.05.011
Morato Torres, C. A., Wassouf, Z., Zafar, F. et al. (2020). The role of alpha-synuclein and other Parkinson’s genes in neurodevelopmental and neurodegenerative disorders. Int J Mol Sci 21, 5724. doi:10.3390/ijms21165724
Müller, T. (2010). New small molecules for the treatment of Parkinson’s disease. Expert Opin Investig Drugs 19, 1077-1086. doi:10.1517/13543784.2010.504711
Nalls, M. A., Blauwendraat, C., Vallerga, C. L. et al. (2019). Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: A meta-analysis of genome-wide association studies. Lancet Neurol 18, 1091-1102. doi:10.1016/s1474-4422(19)30320-5
Napoli, A. and Obeid, I. (2016). Comparative analysis of human and rodent brain primary neuronal culture spontaneous activity using micro-electrode array technology. J Cell Biochem 117, 559-565. doi:10.1002/jcb.25312
Nickels, S. L., Modamio, J., Mendes-Pinheiro, B. et al. (2020). Reproducible generation of human midbrain organoids for in vitro modeling of Parkinson’s disease. Stem Cell Res 46, 101870. doi:10.1016/j.scr.2020.101870
Nido, G. S., Dick, F., Toker, L. et al. (2020). Common gene expression signatures in Parkinson’s disease are driven by changes in cell composition. Acta Neuropathol Commun 8, 55. doi:10.1186/s40478-020-00932-7
NRC (2007). Toxicity Testing in the 21st Century: A Vision and a Strategy. Washington, DC, USA: The National Academies Press. doi:10.17226/11970
Oliveira, L. M. A., Gasser, T., Edwards, R. et al. (2021). Alpha-synuclein research: Defining strategic moves in the battle against Parkinson’s disease. NPJ Parkinsons Dis 7, 65. doi:10.1038/s41531-021-00203-9
Orozco, J. L., Valderrama-Chaparro, J. A., Pinilla-Monsalve, G. D. et al. (2020). Parkinson’s disease prevalence, age distribution and staging in Colombia. Neurol Int 12, 8401. doi:10.4081/ni.2020.8401
Pahuja, G., Nagabhushan, T. N. and Prasad, B. (2020). Early detection of Parkinson’s disease by using SPECT imaging and biomarkers. J Intell Syst 29, 1329-1344. doi:10.1515/jisys-2018-0261
Paini, A., Campia, I., Cronin, M. T. D. et al. (2021). Towards a qAOP framework for predictive toxicology – Linking data to decisions. Comput Toxicol 21, 100195. doi:10.1016/j.comtox.2021.100195
Paiva, I., Pinho, R., Pavlou, M. A. et al. (2017). Sodium butyrate rescues dopaminergic cells from alpha-synuclein-induced transcriptional deregulation and DNA damage. Hum Mol Genet 26, 2231-2246. doi:10.1093/hmg/ddx114
Pamies, D. and Hartung, T. (2017). 21st century cell culture for 21st century toxicology. Chem Res Toxicol 30, 43-52. doi:10.1021/acs.chemrestox.6b00269
Pediaditakis, I., Kodella, K. R., Manatakis, D. V. et al. (2021). Modeling alpha-synuclein pathology in a human brain-chip to assess blood-brain barrier disruption. Nat Commun 12, 5907. doi:10.1038/s41467-021-26066-5
Peters, S., Walker, D., Miller, G. et al. (2019). O6e.4 metabolome and exposome profiling: New opportunities to study risk factors for Parkinson’s disease. J Occup Environ Med 76, A60-A60. doi:10.1136/OEM-2019-EPI.161
Picollet-D’hahan, N., Zuchowska, A., Lemeunier, I. et al. (2021). Multiorgan-on-a-chip: A systemic approach to model and decipher inter-organ communication. Trends Biotechnol 39, 788-810. doi:10.1016/j.tibtech.2020.11.014
Pistollato, F., Cavanaugh, S. E. and Chandrasekera, P. C. (2015). A human-based integrated framework for Alzheimer’s disease research. J Alzheimers Dis 47, 857-868. doi:10.3233/JAD-150281
Pistollato, F., Ohayon, E. L., Lam, A. et al. (2016). Alzheimer disease research in the 21st century: Past and current failures, new perspectives and funding priorities. Oncotarget 7, 38999-39016. doi:10.18632/oncotarget.9175
Pistollato, F., Bernasconi, C., McCarthy, J. et al. (2020). Alzheimer’s disease, and breast and prostate cancer research: Translational failures and the importance to monitor outputs and impact of funded research. Animals (Basel) 10, 1194. doi:10.3390/ani10071194
Posavi, M., Diaz-Ortiz, M., Liu, B. et al. (2019). Characterization of Parkinson’s disease using blood-based biomarkers: A multicohort proteomic analysis. PLoS Med 16, e1002931. doi:10.1371/journal.pmed.1002931
Potashkin, J. A., Blume, S. R. and Runkle, N. K. (2011). Limitations of animal models of Parkinson’s disease. Parkinsons Dis 2011, 658083. doi:10.4061/2011/658083
Pound, P. and Ritskes-Hoitinga, M. (2018). Is it possible to overcome issues of external validity in preclinical animal research? Why most animal models are bound to fail. J Transl Med 16, 304. doi:10.1186/s12967-018-1678-1
Pound, P. (2020). Are animal models needed to discover, develop and test pharmaceutical drugs for humans in the 21st century? Animals 10, 2455. doi:10.3390/ani10122455
Redenšek, S., Dolžan, V. and Kunej, T. (2018). From genomics to omics landscapes of Parkinson’s disease: Revealing the molecular mechanisms. Omics 22, 1-16. doi:10.1089/omi.2017.0181
Reiner, O., Sapir, T. and Parichha, A. (2021). Using multi-organ culture systems to study Parkinson’s disease. Mol Psychiatry 26, 725-735. doi:10.1038/s41380-020-00936-8
Reynolds, R. H., Botía, J., Nalls, M. A. et al. (2019). Moving beyond neurons: The role of cell type-specific gene regulation in Parkinson’s disease heritability. NPJ Parkinsons Dis 5, 6. doi:10.1038/s41531-019-0076-6
Rich, S., Moradi Chameh, H., Sekulic, V. et al. (2020). Modeling reveals human-rodent differences in H-current kinetics influencing resonance in cortical layer 5 neurons. Cereb Cortex 31, 845-872. doi:10.1093/cercor/bhaa261
Roberts, P., Spiros, A. and Geerts, H. (2016). A humanized clinically calibrated quantitative systems pharmacology model for hypokinetic motor symptoms in Parkinson’s disease. Front Pharmacol 7, 6. doi:10.3389/fphar.2016.00006
Romano, S., Savva, G. M., Bedarf, J. R. et al. (2021). Meta-analysis of the Parkinson’s disease gut microbiome suggests alterations linked to intestinal inflammation. NPJ Parkinsons Dis 7, 27. doi:10.1038/s41531-021-00156-z
Rotunno, M. S., Lane, M., Zhang, W. et al. (2020). Cerebrospinal fluid proteomics implicates the granin family in Parkinson’s disease. Sci Rep 10, 2479. doi:10.1038/s41598-020-59414-4
Saeed, U., Compagnone, J., Aviv, R. I. et al. (2017). Imaging biomarkers in Parkinson’s disease and parkinsonian syndromes: Current and emerging concepts. Transl Neurodegener 6, 8. doi:10.1186/s40035-017-0076-6
Scheperjans, F., Derkinderen, P. and Borghammer, P. (2018). The gut and Parkinson’s disease: Hype or hope? J Parkinsons Dis 8, S31-S39. doi:10.3233/jpd-181477
Schildknecht, S., Pöltl, D., Nagel, D. M. et al. (2009). Requirement of a dopaminergic neuronal phenotype for toxicity of low concentrations of 1-methyl-4-phenylpyridinium to human cells. Toxicol Appl Pharmacol 241, 23-35. doi:10.1016/j.taap.2009.07.027
Schildknecht, S., Gerding, H. R., Karreman, C. et al. (2013a). Oxidative and nitrative alpha-synuclein modifications and proteostatic stress: Implications for disease mechanisms and interventions in synucleinopathies. J Neurochem 125, 491-511. doi:10.1111/jnc.12226
Schildknecht, S., Karreman, C., Pöltl, D. et al. (2013b). Generation of genetically-modified human differentiated cells for toxicological tests and the study of neurodegenerative diseases. ALTEX 30, 427-444. doi:10.14573/altex.2013.4.427
Schildknecht, S., Pape, R., Meiser, J. et al. (2015). Preferential extracellular generation of the active parkinsonian toxin MPP+ by transporter-independent export of the intermediate MPDP+. Antioxid Redox Signal 23, 1001-1016. doi:10.1089/ars.2015.6297
Schildknecht, S., Di Monte, D. A., Pape, R. et al. (2017). Tipping points and endogenous determinants of nigrostriatal degeneration by MPTP. Trends Pharmacol Sci 38, 541-555. doi:10.1016/j.tips.2017.03.010
Scholz, D., Pöltl, D., Genewsky, A. et al. (2011). Rapid, complete and large-scale generation of post-mitotic neurons from the human LUHMES cell line. J Neurochem 119, 957-971. doi:10.1111/j.1471-4159.2011.07255.x
Schwamborn, J. C. (2018). Is Parkinson’s disease a neurodevelopmental disorder and will brain organoids help us to understand it? Stem Cells Dev 27, 968-975. doi:10.1089/scd.2017.0289
Simon, D. K., Tanner, C. M. and Brundin, P. (2020). Parkinson disease epidemiology, pathology, genetics, and pathophysiology. Clin Geriatr Med 36, 1-12. doi:10.1016/j.cger.2019.08.002
Sinclair, E., Trivedi, D. K., Sarkar, D. et al. (2021). Metabolomics of sebum reveals lipid dysregulation in Parkinson’s disease. Nat Commun 12, 1592. doi:10.1038/s41467-021-21669-4
Smedinga, M., Darweesh, S. K. L., Bloem, B. R. et al. (2021). Towards early disease modification of Parkinson’s disease: A review of lessons learned in the Alzheimer field. J Neurol 268, 724-733. doi:10.1007/s00415-020-10162-5
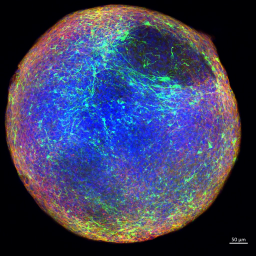
Smirnova, L., Harris, G., Delp, J. et al. (2016). A LUHMES 3D dopaminergic neuronal model for neurotoxicity testing allowing long-term exposure and cellular resilience analysis. Arch Toxicol 90, 2725-2743. doi:10.1007/s00204-015-1637-z
Smits, L. M., Reinhardt, L., Reinhardt, P. et al. (2019). Modeling Parkinson’s disease in midbrain-like organoids. NPJ Parkinsons Dis 5, 5. doi:10.1038/s41531-019-0078-4
Smits, L. M. and Schwamborn, J. C. (2020). Midbrain organoids: A new tool to investigate Parkinson’s disease. Front Cell Dev Biol 8, 359. doi:10.3389/fcell.2020.00359
Tan, A. H., Chong, C. W., Lim, S. Y. et al. (2021). Gut microbial ecosystem in Parkinson disease: New clinicobiological insights from multi-omics. Ann Neurol 89, 546-559. doi:10.1002/ana.25982
Terron, A., Bal-Price, A., Paini, A. et al. (2018). An adverse outcome pathway for parkinsonian motor deficits associated with mitochondrial complex I inhibition. Arch Toxicol 92, 41-82. doi:10.1007/s00204-017-2133-4
Theisen, F., Leda, R., Pozorski, V. et al. (2017). Evaluation of striatonigral connectivity using probabilistic tractography in Parkinson’s disease. Neuroimage Clin 16, 557-563. doi:10.1016/j.nicl.2017.09.009
Trapecar, M., Wogram, E., Svoboda, D. et al. (2021). Human physiomimetic model integrating microphysiological systems of the gut, liver, and brain for studies of neurodegenerative diseases. Sci Adv 7, eabd1707. doi:10.1126/sciadv.abd1707
Troisi, J., Landolfi, A., Vitale, C. et al. (2019). A metabolomic signature of treated and drug-naïve patients with Parkinson’s disease: A pilot study. Metabolomics 15, 90. doi:10.1007/s11306-019-1554-x
Veitch, D. P., Weiner, M. W., Aisen, P. S. et al. (2021). Using the Alzheimer’s disease neuroimaging initiative to improve early detection, diagnosis, and treatment of Alzheimer’s disease. Alzheimers Dement 18, 824-857. doi:10.1002/alz.12422
Werner, C. J., Heyny-von Haussen, R., Mall, G. et al. (2008). Proteome analysis of human substantia nigra in Parkinson’s disease. Proteome Sci 6, 8. doi:10.1186/1477-5956-6-8
Wu, Y., Le, W. and Jankovic, J. (2011). Preclinical biomarkers of Parkinson disease. Arch Neurol 68, 22-30. doi:10.1001/archneurol.2010.321
Zanetti, C., Spitz, S., Berger, E. et al. (2021). Monitoring the neurotransmitter release of human midbrain organoids using a redox cycling microsensor as a novel tool for personalized Parkinson’s disease modelling and drug screening. Analyst 146, 2358-2367. doi:10.1039/D0AN02206C
Zeiss, C. J., Allore, H. G. and Beck, A. P. (2017). Established patterns of animal study design undermine translation of disease-modifying therapies for Parkinson’s disease. PLoS One 12, e0171790. doi:10.1371/journal.pone.0171790
Zhang, X.-M., Yin, M. and Zhang, M.-h. (2014). Cell-based assays for Parkinson’s disease using differentiated human luhmes cells. Acta Pharmacol Sin 35, 945-956. doi:10.1038/aps.2014.36
Zhang, Y. and Burock, M. A. (2020). Diffusion tensor imaging in Parkinson’s disease and parkinsonian syndrome: A systematic review. Front Neurol 11, 531993. doi:10.3389/fneur.2020.531993