Application of immunocompetent microphysiological systems in drug development: Current perspective and recommendations
Main Article Content
Abstract
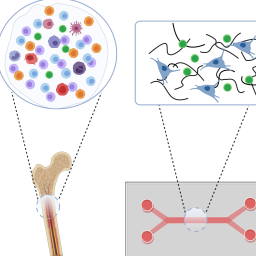
Immune responses are heavily involved in the regulation and pathogenesis of human diseases, including infectious diseases, inflammatory and autoimmune conditions, cancer, neurological disorders, and cardiometabolic syndromes. The immune system is considered a double-edged sword serving as a powerful host defense mechanism against infection and cancerous cells and causing detrimental tissue damage when the immune response is exaggerated or uncontrollable. One of the challenges in studying the efficacy and toxicity of drugs that target or modulate the immune system is the lack of suitable preclinical human models that are predictive of human response. Recent advancements in human microphysiological systems (MPS) have provided a promising in vitro platform to evaluate the response of immune organs ex vivo, to investigate the interaction of immune cells with non-lymphoid tissue cells, and to reduce the reliance on animals in preclinical studies. The development, regulation, trafficking, and responses of immune cells have been extensively studied in preclinical animal models and clinically, providing a wealth of knowledge by which to evaluate new in vitro models. Therefore, the application of immunocompetent MPS in drug discovery and development should first verify that the immune response in an MPS model recapitulates the complexity of the human immune physiology. This manuscript reviews biological functions of immune organ systems and tissue-resident immune cells and discusses contexts-of-use for commonly used immunocompetent and immune organ MPS models. Current perspective and recommendations are provided to guide the continued development of immune organ and immunocompetent MPS models and their application in drug discovery and development.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Articles are distributed under the terms of the Creative Commons Attribution 4.0 International license (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is appropriately cited (CC-BY). Copyright on any article in ALTEX is retained by the author(s).
Abaci, H. E. and Shuler, M. L. (2015). Human-on-a-chip design strategies and principles for physiologically based pharmacokinetics/pharmacodynamics modeling. Integr Biol (Camb) 7, 383-391. doi:10.1039/c4ib00292j
Ainslie, G. R., Davis, M., Ewart, L. et al. (2019). Microphysiological lung models to evaluate the safety of new pharmaceutical modalities: A biopharmaceutical perspective. Lab Chip 19, 3152-3161. doi:10.1039/c9lc00492k
Allen, T. M., Brehm, M. A., Bridges, S. et al. (2019). Humanized immune system mouse models: Progress, challenges and opportunities. Nat Immunol 20, 770-774. doi:10.1038/s41590-019-0416-z
Allwardt, V., Ainscough, A. J., Viswanathan, P. et al. (2020). Translational roadmap for the organs-on-a-chip industry toward broad adoption. Bioengineering (Basel) 7, 112. doi:10.3390/bioengineering7030112
Ambrosini, Y. M., Shin, W., Min, S. et al. (2020). Microphysiological engineering of immune responses in intestinal inflammation. Immune Netw 20, e13. doi:10.4110/in.2020.20.e13
Anderson, G. and Jenkinson, E. J. (2007a). Fetal thymus organ culture. CSH Protoc 2007, pdb prot4808. doi:10.1101/pdb.prot4808
Anderson, G. and Jenkinson, E. J. (2007b). Investigating central tolerance with reaggregate thymus organ cultures. Meth Mol Biol 380, 185-196. doi:10.1007/978-1-59745-395-0_11
Ando, Y., Siegler, E. L., Ta, H. P. et al. (2019). Evaluating CAR-T cell therapy in a hypoxic 3D tumor model. Adv Healthc Mater 8, e1900001. doi:10.1002/adhm.201900001
Atkins, J. T., George, G. C., Hess, K. et al. (2020). Pre-clinical animal models are poor predictors of human toxicities in phase 1 oncology clinical trials. Br J Cancer 123, 1496-1501. doi:10.1038/s41416-020-01033-x
Ayuso, J. M., Truttschel, R., Gong, M. M. et al. (2019). Evaluating natural killer cell cytotoxicity against solid tumors using a microfluidic model. Oncoimmunology 8, 1553477. doi:10.1080/2162402X.2018.1553477
Bachiller, S., Jimenez-Ferrer, I., Paulus, A. et al. (2018). Microglia in neurological diseases: A road map to brain-disease dependent-inflammatory response. Front Cell Neurosci 12, 488. doi:10.3389/fncel.2018.00488
Balogh Sivars, K., Sivars, U., Hornberg, E. et al. (2018). A 3D human airway model enables prediction of respiratory toxicity of inhaled drugs in vitro. Toxicol Sci 162, 301-308. doi:10.1093/toxsci/kfx255
Bar-Ephraim, Y. E., Kretzschmar, K. and Clevers, H. (2020). Organoids in immunological research. Nat Rev Immunol 20, 279-293. doi:10.1038/s41577-019-0248-y
Baran, S. W., Brown, P. C., Baudy, A. R. et al. (2022). Perspectives on the evaluation and adoption of complex in vitro models in drug development: Workshop with the FDA and the pharmaceutical industry (IQ MPS affiliate). ALTEX 39, 297-314. doi:10.14573/altex.2112203
Barrile, R., van der Meer, A. D., Park, H. et al. (2018). Organ-on-chip recapitulates thrombosis induced by an anti-CD154 monoclonal antibody: Translational potential of advanced microengineered systems. Clin Pharmacol Ther 104, 1240-1248. doi:10.1002/cpt.1054
Bartkowiak, T., Jaiswal, A. R., Ager, C. R. et al. (2018). Activation of 4-1BB on liver myeloid cells triggers hepatitis via an interleukin-27-dependent pathway. Clin Cancer Res 24, 1138-1151. doi:10.1158/1078-0432.CCR-17-1847
Baudy, A. R., Otieno, M. A., Hewitt, P. et al. (2020). Liver microphysiological systems development guidelines for safety risk assessment in the pharmaceutical industry. Lab Chip 20, 215-225. doi:10.1039/c9lc00768g
Bejarano, L., Jordao, M. J. C. and Joyce, J. A. (2021). Therapeutic targeting of the tumor microenvironment. Cancer Discov 11, 933-959. doi:10.1158/2159-8290.CD-20-1808
Benam, K. H., Villenave, R., Lucchesi, C. et al. (2016). Small airway-on-a-chip enables analysis of human lung inflammation and drug responses in vitro. Nat Methods 13, 151-157. doi:10.1038/nmeth.3697
Bhattacharya, S., Calar, K. and de la Puente, P. (2020). Mimicking tumor hypoxia and tumor-immune interactions employing three-dimensional in vitro models. J Exp Clin Cancer Res 39, 75. doi:10.1186/s13046-020-01583-1
Birmingham, K. G., O’Melia, M. J., Bordy, S. et al. (2020). Lymph node subcapsular sinus microenvironment-on-a-chip modeling shear flow relevant to lymphatic metastasis and immune cell homing. iScience 23, 101751. doi:10.1016/j.isci.2020.101751
Bock, S., Said, A., Muller, G. et al. (2018). Characterization of reconstructed human skin containing Langerhans cells to monitor molecular events in skin sensitization. Toxicol In Vitro 46, 77-85. doi:10.1016/j.tiv.2017.09.019
Boda, B., Benaoudia, S., Huang, S. et al. (2018). Antiviral drug screening by assessing epithelial functions and innate immune responses in human 3D airway epithelium model. Antiviral Res 156, 72-79. doi:10.1016/j.antiviral.2018.06.007
Bredenkamp, N., Ulyanchenko, S., O’Neill, K. E. et al. (2014). An organized and functional thymus generated from FOXN1-reprogrammed fibroblasts. Nat Cell Biol 16, 902-908. doi:10.1038/ncb3023
Bruce, A., Evans, R., Mezan, R. et al. (2015). Three-dimensional microfluidic tri-culture model of the bone marrow microenvironment for study of acute lymphoblastic leukemia. PLoS One 10, e0140506. doi:10.1371/journal.pone.0140506
Buela, K. A., Omenetti, S. and Pizarro, T. T. (2015). Cross-talk between type 3 innate lymphoid cells and the gut microbiota in inflammatory bowel disease. Curr Opin Gastroenterol 31, 449-455. doi:10.1097/MOG.0000000000000217
Butlen-Ducuing, F., Petavy, F., Guizzaro, L. et al. (2016). Regulatory watch: Challenges in drug development for central nervous system disorders: A European medicines agency perspective. Nat Rev Drug Discov 15, 813-814. doi:10.1038/nrd.2016.237
Candini, O., Grisendi, G., Foppiani, E. M. et al. (2019). A novel 3D in vitro platform for pre-clinical investigations in drug testing, gene therapy, and immuno-oncology. Sci Rep 9, 7154. doi:10.1038/s41598-019-43613-9
Chandorkar, P., Posch, W., Zaderer, V. et al. (2017). Fast-track development of an in vitro 3D lung/immune cell model to study aspergillus infections. Sci Rep 7, 11644. doi:10.1038/s41598-017-11271-4
Chau, D. Y., Johnson, C., MacNeil, S. et al. (2013). The development of a 3D immunocompetent model of human skin. Biofabrication 5, 035011. doi:10.1088/1758-5082/5/3/035011
Chou, D. B., Frismantas, V., Milton, Y. et al. (2020). On-chip recapitulation of clinical bone marrow toxicities and patient-specific pathophysiology. Nat Biomed Eng 4, 394-406. doi:10.1038/s41551-019-0495-z
Collinge, M., Cole, S. H., Schneider, P. A. et al. (2010). Human lymphocyte activation assay: An in vitro method for predictive immunotoxicity testing. J Immunotoxicol 7, 357-366. doi:10.3109/1547691X.2010.523881
Condon, T. V., Sawyer, R. T., Fenton, M. J. et al. (2011). Lung dendritic cells at the innate-adaptive immune interface. J Leukoc Biol 90, 883-895. doi:10.1189/jlb.0311134
Corsini, S. and Roggen, E. L. (2017). Overview of in vitro assessment of immunotoxicity. Curr Opin Toxicol 5, 13-18. doi:10.1016/j.cotox.2017.06.016
Costa, P. F., Albers, H. J., Linssen, J. E. A. et al. (2017). Mimicking arterial thrombosis in a 3D-printed microfluidic in vitro vascular model based on computed tomography angiography data. Lab Chip 17, 2785-2792. doi:10.1039/c7lc00202e
Datta, P., Dey, M., Ataie, Z. et al. (2020). 3D bioprinting for reconstituting the cancer microenvironment. NPJ Precis Oncol 4, 18. doi:10.1038/s41698-020-0121-2
Davies, P. F., Civelek, M., Fang, Y. et al. (2013). The atherosusceptible endothelium: Endothelial phenotypes in complex haemodynamic shear stress regions in vivo. Cardiovasc Res 99, 315-327. doi:10.1093/cvr/cvt101
Delannoy, E., Tellier, G., Cholet, J. et al. (2022). Multi-layered human blood vessels-on-chip design using double viscous finger patterning. Biomedicines 10, 797. doi:10.3390/biomedicines10040797
Denayer, T., Stohr, T. and Van Roy, M. (2014). Animal models in translational medicine: Validation and prediction. New Horiz Transl Med 2, 5-11. doi:10.1016/j.nhtm.2014.08.001
Deng, J., Wei, W., Chen, Z. et al. (2019). Engineered liver-on-a-chip platform to mimic liver functions and its biomedical applications: A review. Micromachines (Basel) 10, 676. doi:10.3390/mi10100676
Di Maggio, N., Piccinini, E., Jaworski, M. et al. (2011). Toward modeling the bone marrow niche using scaffold-based 3D culture systems. Biomaterials 32, 321-329. doi:10.1016/j.biomaterials.2010.09.041
Dupuy, A., Hagimola, L., Mgaieth, N. S. A. et al. (2021). Thromboinflammation model-on-a-chip by whole blood microfluidics on fixed human endothelium. Diagnostics (Basel) 11, 203. doi:10.3390/diagnostics11020203
Eastwood, D., Findlay, L., Poole, S. et al. (2010). Monoclonal antibody TGN1412 trial failure explained by species differences in CD28 expression on CD4+ effector memory T-cells. Br J Pharmacol 161, 512-526. doi:10.1111/j.1476-5381.2010.00922.x
Ehrlich, A., Duche, D., Ouedraogo, G. et al. (2019). Challenges and opportunities in the design of liver-on-chip microdevices. Annu Rev Biomed Eng 21, 219-239. doi:10.1146/annurev-bioeng-060418-052305
Esch, M. B., Smith, A. S., Prot, J. M. et al. (2014). How multi-organ microdevices can help foster drug development. Adv Drug Deliv Rev 69-70, 158-169. doi:10.1016/j.addr.2013.12.003
Friberg, L. E., Sandstrom, M. and Karlsson, M. O. (2010). Scaling the time-course of myelosuppression from rats to patients with a semi-physiological model. Invest New Drugs 28, 744-753. doi:10.1007/s10637-009-9308-7
Germolec, D., Luebke, R., Rooney, A. et al. (2017). Immunotoxicology: A brief history, current status and strategies for future immunotoxicity assessment. Curr Opin Toxicol 5, 55-59. doi:10.1016/j.cotox.2017.08.002
Giese, C., Lubitz, A., Demmler, C. D. et al. (2010). Immunological substance testing on human lymphatic micro-organoids in vitro. J Biotechnol 148, 38-45. doi:10.1016/j.jbiotec.2010.03.001
Goebeler, M. E. and Bargou, R. C. (2020). T cell-engaging therapies – Bites and beyond. Nat Rev Clin Oncol 17, 418-434. doi:10.1038/s41571-020-0347-5
Goyal, G., Prabhala, P., Mahajan, G. et al. (2021). Lymph follicle formation and human vaccination responses reconstituted in an organ-on-a-chip. bioRxiv, preprint. doi:10.1101/806505
Groell, F., Jordan, O. and Borchard, G. (2018). In vitro models for immunogenicity prediction of therapeutic proteins. Eur J Pharm Biopharm 130, 128-142. doi:10.1016/j.ejpb.2018.06.008
Hardwick, R. N., Betts, C. J., Whritenour, J. et al. (2020). Drug-induced skin toxicity: Gaps in preclinical testing cascade as opportunities for complex in vitro models and assays. Lab Chip 20, 199-214. doi:10.1039/c9lc00519f
Holgate, S. T. (2012). Innate and adaptive immune responses in asthma. Nat Med 18, 673-683. doi:10.1038/nm.2731
Hosseini, V., Mallone, A., Nasrollahi, F. et al. (2021). Healthy and diseased in vitro models of vascular systems. Lab Chip 21, 641-659. doi:10.1039/d0lc00464b
Houshmand, M., Soleimani, M., Atashi, A. et al. (2017). Mimicking the acute myeloid leukemia niche for molecular study and drug screening. Tissue Eng Part C Methods 23, 72-85. doi:10.1089/ten.TEC.2016.0404
Hussaini, S. H. and Farrington, E. A. (2007). Idiosyncratic drug-induced liver injury: An overview. Expert Opin Drug Saf 6, 673-684. doi:10.1517/14740338.6.6.673
ICH – International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (2005). ICH S8: Immunotoxicology Studies for Human Pharmaceuticals – Step 5.
ICH (2013a). ICH M3(R2): Non-Clinical Safety Studies for the Conduct of Human Clinical Trials for Pharmaceuticals – Step 5.
ICH (2013b). ICH S9: Non-Clinical Evaluation for Anticancer Pharmaceuticals. Step 5.
Ishiguro, T., Sano, Y., Komatsu, S. I. et al. (2017). An anti-glypican 3/CD3 bispecific T cell-redirecting antibody for treatment of solid tumors. Sci Transl Med 9, eaal4291. doi:10.1126/scitranslmed.aal4291
Jacob, F., Salinas, R. D., Zhang, D. Y. et al. (2020). A patient-derived glioblastoma organoid model and biobank recapitulates inter- and intra-tumoral heterogeneity. Cell 180, 188-204.e122. doi:10.1016/j.cell.2019.11.036
Jagadeesan, S., Workman, M. J., Herland, A. et al. (2020). Generation of a human iPSC-based blood-brain barrier chip. J Vis Exp, e60925. doi:10.3791/60925
Jain, A., van der Meer, A. D., Papa, A. L. et al. (2016). Assessment of whole blood thrombosis in a microfluidic device lined by fixed human endothelium. Biomed Microdevices 18, 73. doi:10.1007/s10544-016-0095-6
Jain, A., Barrile, R., van der Meer, A. D. et al. (2018). Primary human lung alveolus-on-a-chip model of intravascular thrombosis for assessment of therapeutics. Clin Pharmacol Ther 103, 332-340. doi:10.1002/cpt.742
Jean, J., Lapointe, M., Soucy, J. et al. (2009). Development of an in vitro psoriatic skin model by tissue engineering. J Dermatol Sci 53, 19-25. doi:10.1016/j.jdermsci.2008.07.009
Kanabekova, P., Kadyrova, A. and Kulsharova, G. (2022). Microfluidic organ-on-a-chip devices for liver disease modeling in vitro. Micromachines (Basel) 13, 428. doi:10.3390/mi13030428
Kandárová, H., Liebsch, M., Schmidt, E. et al. (2006). Assessment of the skin irritation potential of chemicals by using the SkinEthic reconstructed human epidermal model and the common skin irritation protocol evaluated in the ECVAM skin irritation validation study. Altern Lab Anim 34, 393-406. doi:10.1177/026119290603400407
Kang, J. H., Super, M., Yung, C. W. et al. (2014). An extracorporeal blood-cleansing device for sepsis therapy. Nat Med 20, 1211-1216. doi:10.1038/nm.3640
Karlmark, K. R., Wasmuth, H. E., Trautwein, C. et al. (2008). Chemokine-directed immune cell infiltration in acute and chronic liver disease. Expert Rev Gastroenterol Hepatol 2, 233-242. doi:10.1586/17474124.2.2.233
Kerns, S. J., Belgur, C., Petropolis, D. et al. (2021). Human immunocompetent organ-on-chip platforms allow safety profiling of tumor-targeted T-cell bispecific antibodies. Elife 10, e67106. doi:10.7554/eLife.67106
Kim, S., Kim, W., Lim, S. et al. (2017). Vasculature-on-a-chip for in vitro disease models. Bioengineering (Basel) 4, 8. doi:10.3390/bioengineering4010008
Kindt, T. J., Osborne, B. A., Goldsby, R. A. et al. (2007). Kuby Immunology. New York, USA: W.H. Freeman.
Korenblat, P., Kerwin, E., Leshchenko, I. et al. (2018). Efficacy and safety of lebrikizumab in adult patients with mild-to-moderate asthma not receiving inhaled corticosteroids. Respir Med 134, 143-149. doi:10.1016/j.rmed.2017.12.006
Kraus, T., Lubitz, A., Schliesser, U. et al. (2019). Evaluation of a 3D human artificial lymph node as test model for the assessment of immunogenicity of protein aggregates. J Pharm Sci 108, 2358-2366. doi:10.1016/j.xphs.2019.02.011
Kubes, P. and Jenne, C. (2018). Immune responses in the liver. Annu Rev Immunol 36, 247-277. doi:10.1146/annurev-immunol-051116-052415
Kumar, D. R., Hanlin, E., Glurich, I. et al. (2010). Virchow’s contribution to the understanding of thrombosis and cellular biology. Clin Med Res 8, 168-172. doi:10.3121/cmr.2009.866
Kwak, B. S., Jin, S.-P. J., King, S. J. et al. (2020). Microfluidic skin chip with vasculature for recapitulating the immune response of the skin tissue. Biotechnol Bioeng 117, 1853-1863. doi:10.1002/bit.27320
Kyewski, B. and Klein, L. (2006). A central role for central tolerance. Annu Rev Immunol 24, 571-606. doi:10.1146/annurev.immunol.23.021704.115601
Lambrecht, B. N., Salomon, B., Klatzmann, D. et al. (1998). Dendritic cells are required for the development of chronic eosinophilic airway inflammation in response to inhaled antigen in sensitized mice. J Immunol 160, 4090-4097.
Lambrecht, B. N. and Hammad, H. (2012a). The airway epithelium in asthma. Nat Med 18, 684-692. doi:10.1038/nm.2737
Lambrecht, B. N. and Hammad, H. (2012b). Lung dendritic cells in respiratory viral infection and asthma: From protection to immunopathology. Annu Rev Immunol 30, 243-270. doi:10.1146/annurev-immunol-020711-075021
Langhans, S. A. (2018). Three-dimensional in vitro cell culture models in drug discovery and drug repositioning. Front Pharmacol 9, 6. doi:10.3389/fphar.2018.00006
Lebrec, H., Molinier, B., Boverhof, D. et al. (2014). The T-cell-dependent antibody response assay in nonclinical studies of pharmaceuticals and chemicals: Study design, data analysis, interpretation. Regul Toxicol Pharmacol 69, 7-21. doi:10.1016/j.yrtph.2014.02.008
Lee, S., Dong, D. X., Jindal, R. et al. (2014). Predicting full thickness skin sensitization using a support vector machine. Toxicol In Vitro 28, 1413-1423. doi:10.1016/j.tiv.2014.07.002
Leenaars, C. H. C., Kouwenaar, C., Stafleu, F. R. et al. (2019). Animal to human translation: A systematic scoping review of reported concordance rates. J Transl Med 17, 223. doi:10.1186/s12967-019-1976-2
Lei, X., Lawrence, M. B. and Dong, C. (1999). Influence of cell deformation on leukocyte rolling adhesion in shear flow. J Biomech Eng 121, 636-643. doi:10.1115/1.2800866
Levesque, M. J. and Nerem, R. M. (1985). The elongation and orientation of cultured endothelial cells in response to shear stress. J Biomech Eng 107, 341-347. doi:10.1115/1.3138567
Liston, A., Humblet-Baron, S., Duffy, D. et al. (2021). Human immune diversity: From evolution to modernity. Nat Immunol 22, 1479-1489. doi:10.1038/s41590-021-01058-1
Liu, Z., Shi, Q., Ding, D. et al. (2011). Translating clinical findings into knowledge in drug safety evaluation – Drug induced liver injury prediction system (DILIps). PLoS Comput Biol 7, e1002310. doi:10.1371/journal.pcbi.1002310
Loessner, D., Stok, K. S., Lutolf, M. P. et al. (2010). Bioengineered 3D platform to explore cell-ECM interactions and drug resistance of epithelial ovarian cancer cells. Biomaterials 31, 8494-8506. doi:10.1016/j.biomaterials.2010.07.064
Louveau, A., Harris, T. H. and Kipnis, J. (2015). Revisiting the mechanisms of CNS immune privilege. Trends Immunol 36, 569-577. doi:10.1016/j.it.2015.08.006
Low, L. A., Mummery, C., Berridge, B. R. et al. (2021). Organs-on-chips: Into the next decade. Nat Rev Drug Discov 20, 345-361. doi:10.1038/s41573-020-0079-3
Lu, R. X. Z., Lai, B. F. L., Rafatian, N. et al. (2022). Vasculature-on-a-chip platform with innate immunity enables identification of angiopoietin-1 derived peptide as a therapeutic for SARS-CoV-2 induced inflammation. Lab Chip 22, 1171-1186. doi:10.1039/d1lc00817j
Luster, M. I., Portier, C., Pait, D. G. et al. (1992). Risk assessment in immunotoxicology. I. Sensitivity and predictability of immune tests. Fundam Appl Toxicol 18, 200-210. doi:10.1016/0272-0590(92)90047-l
MacArthur Clark, J. (2018). The 3Rs in research: A contemporary approach to replacement, reduction and refinement. Br J Nutr 120, S1-S7. doi:10.1017/S0007114517002227
Mahalingaiah, P. K., Palenski, T. and Van Vleet, T. R. (2018). An in vitro model of hematotoxicity: Differentiation of bone marrow-derived stem/progenitor cells into hematopoietic lineages and evaluation of lineage-specific hematotoxicity. Curr Protoc Toxicol 76, e45. doi:10.1002/cptx.45
Malek, A. M., Alper, S. L. and Izumo, S. (1999). Hemodynamic shear stress and its role in atherosclerosis. JAMA 282, 2035-2042. doi:10.1001/jama.282.21.2035
Manson, M. L., Safholm, J., James, A. et al. (2020). IL-13 and IL-4, but not IL -5 nor IL -17A, induce hyperresponsiveness in isolated human small airways. J Allergy Clin Immunol 145, 808-817 e802. doi:10.1016/j.jaci.2019.10.037
Martinod, K. and Wagner, D. D. (2014). Thrombosis: Tangled up in nets. Blood 123, 2768-2776. doi:10.1182/blood-2013-10-463646
Marx, U., Akabane, T., Andersson, T. B. et al. (2020). Biology-inspired microphysiological systems to advance patient benefit and animal welfare in drug development. ALTEX 37, 365-394. doi:10.14573/altex.2001241
Matejuk, A. (2018). Skin immunity. Arch Immunol Ther Exp (Warsz) 66, 45-54. doi:10.1007/s00005-017-0477-3
Mathur, T., Singh, K. A., R Pandian, N. K. et al. (2019). Organ-on-chips made of blood: Endothelial progenitor cells from blood reconstitute vascular thromboinflammation in vessel-chips. Lab Chip 19, 2500-2511. doi:10.1039/c9lc00469f
Maurer, M., Gresnigt, M. S., Last, A. et al. (2019). A three-dimensional immunocompetent intestine-on-chip model as in vitro platform for functional and microbial interaction studies. Biomaterials 220, 119396. doi:10.1016/j.biomaterials.2019.119396
McEver, R. P. and Zhu, C. (2010). Rolling cell adhesion. Annu Rev Cell Dev Biol 26, 363-396. doi:10.1146/annurev.cellbio.042308.113238
Mestas, J. and Hughes, C. C. (2004). Of mice and not men: Differences between mouse and human immunology. J Immunol 172, 2731-2738. doi:10.4049/jimmunol.172.5.2731
Mitra, B., Jindal, R., Lee, S. et al. (2013). Microdevice integrating innate and adaptive immune responses associated with antigen presentation by dendritic cells. RSC Adv 3, 16002-16010. doi:10.1039/C3RA41308J
Monticello, T. M., Jones, T. W., Dambach, D. M. et al. (2017). Current nonclinical testing paradigm enables safe entry to first-in-human clinical trials: The IQ consortium nonclinical to clinical translational database. Toxicol Appl Pharmacol 334, 100-109. doi:10.1016/j.taap.2017.09.006
Morsink, M. A. J., Willemen, N. G. A., Leijten, J. et al. (2020). Immune organs and immune cells on a chip: An overview of biomedical applications. Micromachines (Basel) 11, 849. doi:10.3390/mi11090849
Moura Rosa, P., Gopalakrishnan, N., Ibrahim, H. et al. (2016). The intercell dynamics of T cells and dendritic cells in a lymph node-on-a-chip flow device. Lab Chip 16, 3728-3740. doi:10.1039/c6lc00702c
Nakano, H., Free, M. E., Whitehead, G. S. et al. (2012). Pulmonary CD103+ dendritic cells prime Th2 responses to inhaled allergens. Mucosal Immunol 5, 53-65. doi:10.1038/mi.2011.47
Okabe, M., Ito, S., Nishio, N. et al. (2015). Thymic epithelial cells induced from pluripotent stem cells by a three-dimensional spheroid culture system regenerates functional T cells in nude mice. Cell Reprogram 17, 368-375. doi:10.1089/cell.2015.0006
Olaharski, A. J., Uppal, H., Cooper, M. et al. (2009). In vitro to in vivo concordance of a high throughput assay of bone marrow toxicity across a diverse set of drug candidates. Toxicol Lett 188, 98-103. doi:10.1016/j.toxlet.2009.03.012
Olson, H., Betton, G., Robinson, D. et al. (2000). Concordance of the toxicity of pharmaceuticals in humans and in animals. Regul Toxicol Pharmacol 32, 56-67. doi:10.1006/rtph.2000.1399
Owens, A. P., 3rd and Mackman, N. (2010). Tissue factor and thrombosis: The clot starts here. Thromb Haemost 104, 432-439. doi:10.1160/TH09-11-0771
Park, J., Wetzel, I., Marriott, I. et al. (2018). A 3D human triculture system modeling neurodegeneration and neuroinflammation in Alzheimer’s disease. Nat Neurosci 21, 941-951. doi:10.1038/s41593-018-0175-4
Pellevoisin, C., Videau, C., Briotet, D. et al. (2018). SkinEthic™ RHE for in vitro evaluation of skin irritation of medical device extracts. Toxicol In Vitro 50, 418-425. doi:10.1016/j.tiv.2018.01.008
Peterson, L. W. and Artis, D. (2014). Intestinal epithelial cells: Regulators of barrier function and immune homeostasis. Nat Rev Immunol 14, 141-153. doi:10.1038/nri3608
Peterson, N. C., Mahalingaiah, P. K., Fullerton, A. et al. (2020). Application of microphysiological systems in biopharmaceutical research and development. Lab Chip 20, 697-708. doi:10.1039/c9lc00962k
Polini, A., Del Mercato, L. L., Barra, A. et al. (2019). Towards the development of human immune-system-on-a-chip platforms. Drug Discov Today 24, 517-525. doi:10.1016/j.drudis.2018.10.003
Poznansky, M. C., Evans, R. H., Foxall, R. B. et al. (2000). Efficient generation of human T cells from a tissue-engineered thymic organoid. Nat Biotechnol 18, 729-734. doi:10.1038/77288
Prantil-Baun, R., Novak, R., Das, D. et al. (2018). Physiologically based pharmacokinetic and pharmacodynamic analysis enabled by microfluidically linked organs-on-chips. Annu Rev Pharmacol Toxicol 58, 37-64. doi:10.1146/annurev-pharmtox-010716-104748
Raic, A., Naolou, T., Mohra, A. et al. (2019). 3D models of the bone marrow in health and disease: Yesterday, today and tomorrow. MRS Commun 9, 37-52. doi:10.1557/mrc.2018.203
Raies, A. B. and Bajic, V. B. (2016). In silico toxicology: Computational methods for the prediction of chemical toxicity. Wiley Interdiscip Rev Comput Mol Sci 6, 147-172. doi:10.1002/wcms.1240
Rajeeva Pandian, N. K., Walther, B. K., Suresh, R. et al. (2020). Microengineered human vein-chip recreates venous valve architecture and its contribution to thrombosis. Small 16, e2003401. doi:10.1002/smll.202003401
Ramadan, Q. and Ting, F. C. (2016). In vitro micro-physiological immune-competent model of the human skin. Lab Chip 16, 1899-1908. doi:10.1039/c6lc00229c
Ramadori, G. and Saile, B. (2004). Inflammation, damage repair, immune cells, and liver fibrosis: Specific or nonspecific, this is the question. Gastroenterology 127, 997-1000. doi:10.1053/j.gastro.2004.07.041
Ramos-Casals, M., Brahmer, J. R., Callahan, M. K. et al. (2020). Immune-related adverse events of checkpoint inhibitors. Nat Rev Dis Primers 6, 38. doi:10.1038/s41572-020-0160-6
Ramot, Y. and Nyska, A. (2007). Drug-induced thrombosis – Experimental, clinical, and mechanistic considerations. Toxicol Pathol 35, 208-225. doi:10.1080/01926230601156237
Ramot, Y., Nyska, A. and Spectre, G. (2013). Drug-induced thrombosis: An update. Drug Saf 36, 585-603. doi:10.1007/s40264-013-0054-6
Raskob, G. E., Hull, R. D. and Buller, H. R. (2018). Chapter 23: Venous Thrombosis. In K. Kaushansky and M. Levi (eds.): Williams Hematology Hemostasis and Thrombosis. McGraw-Hill Education.
Rigat-Brugarolas, L. G., Elizalde-Torrent, A., Bernabeu, M. et al. (2014). A functional microengineered model of the human splenon-on-a-chip. Lab Chip 14, 1715-1724. doi:10.1039/c3lc51449h
Robert, C., Schachter, J., Long, G. V. et al. (2015). Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med 372, 2521-2532. doi:10.1056/NEJMoa1503093
Robinson, J. H. and Owen, J. J. (1977). Generation of T-cell function in organ culture of foetal mouse thymus. II. Mixed lymphocyte culture reactivity. Clin Exp Immunol 27, 322-327.
Ropke, C. (1997). Thymic epithelial cell culture. Microsc Res Tech 38, 276-286. doi:10.1002/(SICI)1097-0029(19970801)38:3<276::AID-JEMT8>3.0.CO;2-K
Sahmoudi, K., Abbassi, H., Bouklata, N. et al. (2018). Immune activation and regulatory T cells in mycobacterium tuberculosis infected lymph nodes. BMC Immunol 19, 33. doi:10.1186/s12865-018-0266-8
Sasserath, T., Rumsey, J. W., McAleer, C. W. et al. (2020). Differential monocyte actuation in a three-organ functional innate immune system-on-a-chip. Adv Sci (Weinh) 7, 2000323. doi:10.1002/advs.202000323
Sato, T., Stange, D. E., Ferrante, M. et al. (2011). Long-term expansion of epithelial organoids from human colon, adenoma, adenocarcinoma, and Barrett’s epithelium. Gastroenterology 141, 1762-1772. doi:10.1053/j.gastro.2011.07.050
Savchenko, A. S., Martinod, K., Seidman, M. A. et al. (2014). Neutrophil extracellular traps form predominantly during the organizing stage of human venous thromboembolism development. J Thromb Haemost 12, 860-870. doi:10.1111/jth.12571
Schnalzger, T. E., de Groot, M. H., Zhang, C. et al. (2019). 3D model for car-mediated cytotoxicity using patient-derived colorectal cancer organoids. EMBO J 38, e100928. doi:10.15252/embj.2018100928
Seet, C. S., He, C., Bethune, M. T. et al. (2017). Generation of mature T cells from human hematopoietic stem and progenitor cells in artificial thymic organoids. Nat Methods 14, 521-530. doi:10.1038/nmeth.4237
Shanti, A., Teo, J. and Stefanini, C. (2018). In vitro immune organs-on-chip for drug development: A review. Pharmaceutics 10, 278. doi:10.3390/pharmaceutics10040278
Shanti, A., Samara, B., Abdullah, A. et al. (2020). Multi-compartment 3D-cultured organ-on-a-chip: Towards a biomimetic lymph node for drug development. Pharmaceutics 12, 464. doi:10.3390/pharmaceutics12050464
Sharifi, F., Htwe, S. S., Righi, M. et al. (2019). A foreign body response-on-a-chip platform. Adv Healthc Mater 8, e1801425. doi:10.1002/adhm.201801425
Shimizu, K., Iyoda, T., Okada, M. et al. (2018). Immune suppression and reversal of the suppressive tumor microenvironment. Int Immunol 30, 445-454. doi:10.1093/intimm/dxy042
Si, L., Bai, H., Rodas, M. et al. (2021). A human-airway-on-a-chip for the rapid identification of candidate antiviral therapeutics and prophylactics. Nat Biomed Eng 5, 815-829. doi:10.1038/s41551-021-00718-9
Sieber, S., Wirth, L., Cavak, N. et al. (2018). Bone marrow-on-a-chip: Long-term culture of human haematopoietic stem cells in a three-dimensional microfluidic environment. J Tissue Eng Regen Med 12, 479-489. doi:10.1002/term.2507
Skaggs, H., Chellman, G. J., Collinge, M. et al. (2019). Comparison of immune system development in nonclinical species and humans: Closing information gaps for immunotoxicity testing and human translatability. Reprod Toxicol 89, 178-188. doi:10.1016/j.reprotox.2019.06.005
Steinway, S. N., Saleh, J., Koo, B. K. et al. (2020). Human microphysiological models of intestinal tissue and gut microbiome. Front Bioeng Biotechnol 8, 725. doi:10.3389/fbioe.2020.00725
Sun, A. and Benet, L. Z. (2020). Late-stage failures of monoclonal antibody drugs: A retrospective case study analysis. Pharmacology 105, 145-163. doi:10.1159/000505379
Sung, J. H., Wang, Y. I., Narasimhan Sriram, N. et al. (2019). Recent advances in body-on-a-chip systems. Anal Chem 91, 330-351. doi:10.1021/acs.analchem.8b05293
Suntharalingam, G., Perry, M. R., Ward, S. et al. (2006). Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med 355, 1018-1028. doi:10.1056/NEJMoa063842
Sura, R., Van Vleet, T. and Berridge, B. R. (2020). Microphysiological systems: A pathologist’s perspective. Vet Pathol 57, 358-368. doi:10.1177/0300985820908794
Sweeney, M. D., Sagare, A. P. and Zlokovic, B. V. (2018). Blood-brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nat Rev Neurol 14, 133-150. doi:10.1038/nrneurol.2017.188
Ta, G. H., Weng, C. F. and Leong, M. K. (2021). In silico prediction of skin sensitization: Quo vadis? Front Pharmacol 12, 655771. doi:10.3389/fphar.2021.655771
Tajima, A., Pradhan, I., Trucco, M. et al. (2016). Restoration of thymus function with bioengineered thymus organoids. Curr Stem Cell Rep 2, 128-139. doi:10.1007/s40778-016-0040-x
Tannenbaum, J. and Bennett, B. T. (2015). Russell and Burch’s 3Rs then and now: The need for clarity in definition and purpose. J Am Assoc Lab Anim Sci 54, 120-132.
Tesmer, L. A., Lundy, S. K., Sarkar, S. et al. (2008). Th17 cells in human disease. Immunol Rev 223, 87-113. doi:10.1111/j.1600-065X.2008.00628.x
Torisawa, Y. S., Mammoto, T., Jiang, E. et al. (2016). Modeling hematopoiesis and responses to radiation countermeasures in a bone marrow-on-a-chip. Tissue Eng Part C Methods 22, 509-515. doi:10.1089/ten.TEC.2015.0507
Travaglini, K. J., Nabhan, A. N., Penland, L. et al. (2020). A molecular cell atlas of the human lung from single-cell RNA sequencing. Nature 587, 619-625. doi:10.1038/s41586-020-2922-4
Tsai, M., Kita, A., Leach, J. et al. (2012). In vitro modeling of the microvascular occlusion and thrombosis that occur in hematologic diseases using microfluidic technology. J Clin Invest 122, 408-418. doi:10.1172/JCI58753
Twomey, L., Wallace, R. G., Cummins, P. M. et al. (2018). Platelets: From formation to function. In F. Lasakosvitsch and S. Dos Anjos Garnes (eds), Homeostasis – An Integrated Vision. InTechOpen. doi:10.5772/intechopen.80924
van den Bogaard, E. H., Tjabringa, G. S., Joosten, I. et al. (2014). Crosstalk between keratinocytes and T cells in a 3D microenvironment: A model to study inflammatory skin diseases. J Invest Dermatol 134, 719-727. doi:10.1038/jid.2013.417
van Langelaar, J., Rijvers, L., Smolders, J. et al. (2020). B and T cells driving multiple sclerosis: Identity, mechanisms and potential triggers. Front Immunol 11, 760. doi:10.3389/fimmu.2020.00760
Vianello, F. and Poznansky, M. C. (2007). Generation of a tissue-engineered thymic organoid. Methods Mol Biol 380, 163-170. doi:10.1007/978-1-59745-395-0_9
Wagar, L. E., Salahudeen, A., Constantz, C. M. et al. (2021). Modeling human adaptive immune responses with tonsil organoids. Nat Med 27, 125-135. doi:10.1038/s41591-020-01145-0
Wallstabe, L., Gottlich, C., Nelke, L. C. et al. (2019). ROR1-CAR T cells are effective against lung and breast cancer in advanced microphysiologic 3D tumor models. JCI Insight 4, e126345. doi:10.1172/jci.insight.126345
Wallstabe, J., Bussemer, L., Groeber-Becker, F. et al. (2020). Inflammation-induced tissue damage mimicking GvHD in human skin models as test-platform for immunotherapeutics. ALTEX 37, 429-440. doi:10.14573/altex.1907181
Wang, M., Yao, L. C., Cheng, M. et al. (2018). Humanized mice in studying efficacy and mechanisms of PD-1-targeted cancer immunotherapy. FASEB J 32, 1537-1549. doi:10.1096/fj.201700740R
Wang, S., Li, J., Wu, S. et al. (2018). Type 3 innate lymphoid cell: A new player in liver fibrosis progression. Clin Sci (Lond) 132, 2565-2582. doi:10.1042/CS20180482
Weaver, J. L., Zadrozny, L. M., Gabrielson, K. et al. (2019). BLT-immune humanized mice as a model for nivolumab-induced immune-mediated adverse events: Comparison of the NOG and NOG-EXL strains. Toxicol Sci 169, 194-208. doi:10.1093/toxsci/kfz045
Wei, Y., Li, Y., Yan, L. et al. (2020). Alterations of gut microbiome in autoimmune hepatitis. Gut 69, 569-577. doi:10.1136/gutjnl-2018-317836
Westein, E., van der Meer, A. D., Kuijpers, M. J. et al. (2013). Atherosclerotic geometries exacerbate pathological thrombus formation poststenosis in a von Willebrand factor-dependent manner. Proc Natl Acad Sci U S A 110, 1357-1362. doi:10.1073/pnas.1209905110
Wikswo, J. P. (2014). The relevance and potential roles of microphysiological systems in biology and medicine. Exp Biol Med (Maywood) 239, 1061-1072. doi:10.1177/1535370214542068
Wu, T., Gao, Y. Y., Su, J. et al. (2021). Three-dimensional bioprinting of artificial ovaries by an extrusion-based method using gelatin-methacryloyl bioink. Climacteric 25, 170-178. doi:10.1080/13697137.2021.1921726
Xiang, Y., Wen, H., Yu, Y. et al. (2020). Gut-on-chip: Recreating human intestine in vitro. J Tissue Eng 11, 2041731420965318. doi:10.1177/2041731420965318
Yadav, N. K., Shukla, P., Omer, A. et al. (2016). Alternative methods in toxicology: CFU assays application, limitation and future prospective. Drug Chem Toxicol 39, 1-12. doi:10.3109/01480545.2014.994217
Yan, H., Semple, K. M., Gonzalez, C. M. et al. (2019). Bone marrow-liver-thymus (BLT) immune humanized mice as a model to predict cytokine release syndrome. Transl Res 210, 43-56. doi:10.1016/j.trsl.2019.04.007
Ye, C., Yang, H., Cheng, M. et al. (2020). A rapid, sensitive, and reproducible in vivo PBMC humanized murine model for determining therapeutic-related cytokine release syndrome. FASEB J 34, 12963-12975. doi:10.1096/fj.202001203R
Yu, Y. R., Hotten, D. F., Malakhau, Y. et al. (2016). Flow cytometric analysis of myeloid cells in human blood, bronchoalveolar lavage, and lung tissues. Am J Respir Cell Mol Biol 54, 13-24. doi:10.1165/rcmb.2015-0146OC
Zhang, J., Liu, Y., Han, X. et al. (2019). Rats provide a superior model of human stress erythropoiesis. Exp Hematol 78, 21-34 e23. doi:10.1016/j.exphem.2019.09.021
Zhang, Y. S., Davoudi, F., Walch, P. et al. (2016). Bioprinted thrombosis-on-a-chip. Lab Chip 16, 4097-4105. doi:10.1039/c6lc00380j
Zhang, Y. S., Oklu, R. and Albadawi, H. (2017). Bioengineered in vitro models of thrombosis: Methods and techniques. Cardiovasc Diagn Ther 7, S329-S335. doi:10.21037/cdt.2017.08.08