Comparing translational success rates across medical research fields - A combined analysis of literature and clinical trial data
Main Article Content
Abstract
Many interventions that show promising results in preclinical development do not pass clinical tests. Part of this may be explained by poor animal-to-human translation. Using animal models with low predictability for humans is neither ethical nor efficient. If translational success shows variation between medical research fields, analyses of common practices in these fields could identify factors contributing to successful translation. We assessed translational success rates in medical research fields using two approaches: through literature and clinical trial registers.
Literature: We comprehensively searched PubMed for pharmacology, neuroscience, cancer research, animal models, clinical trials, and translation. After screening, 117 review papers were included in this scoping review. Translational success rates were not different within pharmacology (72%), neuroscience (62%), and cancer research (69%).
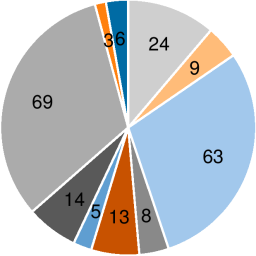
Clinical trials: The fraction of phase-2 clinical trials with a positive outcome was used as a proxy (i.e., an indirect resemblance measure) for translational success. Trials were retrieved from the WHO trial register and categorized into medical research fields following the international classification of disease (ICD-10). Of the phase-2 trials analyzed, 65.2% were successful. Fields with the highest success rates were disorders of lipoprotein metabolism (86.0%) and epilepsy (85.0%). Fields with the lowest success rates were schizophrenia (45.4%) and pancreatic cancer (46.0%).
Our combined analyses suggest relevant differences in success rates between medical research fields. Based on the clinical trials, comparisons of practice, e.g., between epilepsy and schizophrenia, might identify factors that influence translational success.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Articles are distributed under the terms of the Creative Commons Attribution 4.0 International license (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is appropriately cited (CC-BY). Copyright on any article in ALTEX is retained by the author(s).
Albersheim, J., Smith, D. W., Pariser, J. J. et al. (2021). The reporting quality of randomized controlled trials and experimental animal studies for urethroplasty. World J Urol 39, 2677-2683. doi:10.1007/s00345-020-03501-8
Azkona, G. and Sanchez-Pernaute, R. (2022). Mice in translational neuroscience: What R we doing? Prog Neurobiol 217 102330. doi:10.1016/j.pneurobio.2022.102330
Bolker, J. A. (2017). Animal models in translational research: Rosetta stone or stumbling block? Bioassays 39. doi:10.1002/bies.201700089
Davies, C., Hamilton, O. K. L., Hooley, M. et al. (2020). Translational neuroscience: The state of the nation (a PhD student perspective). Brain Commun 2, fcaa038. doi:10.1093/braincomms/fcaa038
Giles, K., Olson, S. H. and Prusiner, S. B. (2017). Developing therapeutics for PrP prion diseases. Cold Spring Harb Perspect Med 7, a023747. doi:10.1101/cshperspect.a023747
Hooijmans, C. R., Tillema, A., Leenaars, M. et al. (2010). Enhancing search efficiency by means of a search filter for finding all studies on animal experimentation in PubMed. Lab Anim 44, 170-175. doi:10.1258/la.2010.009117
Hyman, S. E. (2012). Revolution stalled. Sci Transl Med 4, 155cm111. doi:10.1126/scitranslmed.3003142
Kola, I. and Landis, J. (2004). Can the pharmaceutical industry reduce attrition rates? Nat Rev Drug Discov 3, 711-715. doi:10.1038/nrd1470
Leenaars, C. H. C., Kouwenaar, C., Stafleu, F. R. et al. (2019). Animal to human translation: A systematic scoping review of reported concordance rates. J Translat Med 17, 223. doi:10.1186/s12967-019-1976-2
McNamara, J. P., Hanigan, M. D. and White, R. R. (2016). Invited review: Experimental design, data reporting, and sharing in support of animal systems modeling research. J Dairy Sci 99, 9355-9371. doi:10.3168/jds.2015-10303
Micheli, L., Ceccarelli, M., D’Andrea, G. et al. (2018). Depression and adult neurogenesis: Positive effects of the antidepressant fluoxetine and of physical exercise. Brain Res Bull 143, 181-193. doi:10.1016/j.brainresbull.2018.09.002
O’Collins, V. E., Macleod, M. R., Donnan, G. A. et al. (2006). 1,026 experimental treatments in acute stroke. Ann Neurol 59, 467-477. doi:10.1002/ana.20741
Sedláková, L., Čertíková Chábová, V., Doleželová, Š. et al. (2017). Renin-angiotensin system blockade alone or combined with ETA receptor blockade: Effects on the course of chronic kidney disease in 5/6 nephrectomized Ren-2 transgenic hypertensive rats. Clin Exp Hypertens 39, 183-195. doi:10.1080/10641963.2016.1235184
van der Mierden, S., Hooijmans, C. R., Tillema, A. H. et al. (2022). Laboratory animals search filter for different literature databases: PubMed, Embase, Web of Science and PsycINFO. Lab Anim 56, 279-286. doi:10.1177/00236772211045485
Wong, B. (2011). Points of view: Color blindness. Nat Meth 8, 441-441. doi:10.1038/nmeth.1618