Qualitative and quantitative concentration-response modelling of gene co-expression networks to unlock hepatotoxic mechanisms for next generation chemical safety assessment
Main Article Content
Abstract
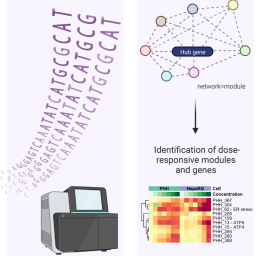
Next generation risk assessment of chemicals revolves around the use of mechanistic information without animal experimentation. In this regard, toxicogenomics has proven to be a useful tool to elucidate the mechanisms underlying the adverse effects of xenobiotics. In the present study, two widely used human hepatocyte culture systems, namely primary human hepatocytes (PHH) and human hepatoma HepaRG cells, were exposed to liver toxicants known to induce liver cholestasis, steatosis, or necrosis. Benchmark concentration (BMC) response modelling was applied to transcriptomics gene co-expression networks (modules) to derive BMCs and to gain mechanistic insight into the hepatotoxic effects. BMCs derived by concentration-response modelling of gene co-expression modules recapitulated concentration-response modelling of individual genes. Although PHH and HepaRG cells showed overlap in the genes and modules deregulated by the liver toxicants, PHH demonstrated a higher responsiveness, based on the lower BMCs of co-regulated gene modules. Such BMCs can be used as transcriptomics points of departure (tPOD) for assessing module-associated cellular (stress) pathways/processes. This approach identified clear tPODs of around maximum systemic concentration (Cmax) levels for the tested drugs, while for cosmetics ingredients the BMCs were 10-100-fold higher than the estimated plasma concentrations. This approach could serve next generation risk assessment practice to identify early responsive modules at low BMCs that could be linked to key events in liver adverse outcome pathways. In turn, this can assist in delineating potential hazards of new test chemicals using in vitro systems and be used in a risk assessment where BMCs are paired with chemical exposure assessment.
Plain language summary
Risk assessment of chemicals has traditionally been focused on animal experiments. In contrast, next generation risk assessment uses biological information obtained from experiments in cell culture models without animals to identify potential hazards. Since the liver is the main target organ of toxicity, many liver cell models have been developed and applied for hazard assessment. In this study, two widely used human liver cell models were exposed to liver toxic chemicals. Biological changes in gene expression were measured in a concentration range to identify the concentration at which a biological response started to be perturbed using a mathematical modelling approach. Genes belonging to the same biological process were linked based on co-expression to derive an average concentration for this process. This animal-free approach could be applied to risk assessment by relating the biological response concentrations to the expected human exposure to identify the potential hazard of test chemicals.
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Articles are distributed under the terms of the Creative Commons Attribution 4.0 International license (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution and reproduction in any medium, provided the original work is appropriately cited (CC-BY). Copyright on any article in ALTEX is retained by the author(s).
AbdulHameed, M. D. M., Pannala, V. R. and Wallqvist, A. (2019). Mining public toxicogenomic data reveals insights and challenges in delineating liver steatosis adverse outcome pathways. Front Genet 10, 1007. doi:10.3389/fgene.2019.01007
Aisenbrey, E. A. and Murphy, W. L. (2020). Synthetic alternatives to Matrigel. Nat Rev Mater 5, 539-551. doi:10.1038/s41578-020-0199-8
Allen, T. E. H., Goodman, J. M., Gutsell, S. et al. (2014). Defining molecular initiating events in the adverse outcome pathway framework for risk assessment. Chem Res Toxicol 27, 2100-2112. doi:10.1021/tx500345j
Andersson, T. B., Kanebratt, K. P. and Kenna, J. G. (2012). The HepaRG cell line: A unique in vitro tool for understanding drug metabolism and toxicology in human. Expert Opin Drug Metab Toxicol 8, 909-920. doi:10.1517/17425255.2012.685159
Arnesdotter, E., Spinu, N., Firman, J. et al. (2021). Derivation, characterisation and analysis of an adverse outcome pathway network for human hepatotoxicity. Toxicology 459, 152856. doi:10.1016/j.tox.2021.152856
Arnesdotter, E., Gijbels, E., dos Santos Rodrigues, B. et al. (2022). Adverse outcome pathways as versatile tools in liver toxicity testing In E. Benfenati (ed.), In Silico Methods for Predicting Drug Toxicity (521-535). Methods in Molecular Biology, Volume 2425. New York, NY, USA: Humana. doi:10.1007/978-1-0716-1960-5_20
Baird, L. and Dinkova-Kostova, A. T. (2011). The cytoprotective role of the Keap1-Nrf2 pathway. Arch Toxicol 85, 241-272. doi:10.1007/s00204-011-0674-5
Barel, G. and Herwig, R. (2018). Network and pathway analysis of toxicogenomics data. Front Genet 9, 484. doi:10.3389/fgene.2018.00484
Barutcu, A. R., Black, M. B. and Nong, A. (2023). Mining toxicogenomic data for dose-responsive pathways: Implications in advancing next-generation risk assessment. Front Toxicol 5, 1272364. doi:10.3389/ftox.2023.1272364
Basili, D., Reynolds, J., Houghton, J. et al. (2022). Latent variables capture pathway-level points of departure in high-throughput toxicogenomic data. Chem Res Toxicol 35, 670-683. doi:10.1021/acs.chemrestox.1c00444
Bechmann, L. P., Hannivoort, R. A., Gerken, G. et al. (2012). The interaction of hepatic lipid and glucose metabolism in liver diseases. J Hepatol 56, 952-964. doi:10.1016/j.jhep.2011.08.025
Begriche, K., Massart, J., Robin, M.-A. et al. (2011). Drug-induced toxicity on mitochondria and lipid metabolism: Mechanistic diversity and deleterious consequences for the liver. J Hepatol 54, 773-794. doi:10.1016/j.jhep.2010.11.006
Bellwon, P., Truisi, G. L., Bois, F. Y. et al. (2015). Kinetics and dynamics of cyclosporine A in three hepatic cell culture systems. Toxicol In Vitro 30, 60-78. doi:10.1016/j.tiv.2015.07.016
Berggren, E., White, A., Ouedraogo, G. et al. (2017). Ab initio chemical safety assessment: A workflow based on exposure considerations and non-animal methods. Comput Toxicol 4, 31-44. doi:10.1016/j.comtox.2017.10.001
Böhme, M., Müller, M., Leier, I. et al. (1994). Cholestasis caused by inhibition of the adenosine triphosphate-dependent bile salt transport in rat liver. Gastroenterology 107, 255-265. doi:10.1016/0016-5085(94)90084-1
Burban, A., Sharanek, A., Guguen-Guillouzo, C. et al. (2018). Endoplasmic reticulum stress precedes oxidative stress in antibiotic-induced cholestasis and cytotoxicity in human hepatocytes. Free Radic Biol Med 115, 166-178. doi:10.1016/j.freeradbiomed.2017.11.017
Callegaro, G., Kunnen, S. J., Trairatphisan, P. et al. (2021). The human hepatocyte TXG-MAPr: Gene co-expression network modules to support mechanism-based risk assessment. Arch Toxicol 95, 3745-3775. doi:10.1007/s00204-021-03141-w
Cao, S. S. and Kaufman, R. J. (2014). Endoplasmic reticulum stress and oxidative stress in cell fate decision and human disease. Antioxid Redox Signal 21, 396-413. doi:10.1089/ars.2014.5851
Chatterjee, S. and Annaert, P. (2018). Drug-induced cholestasis: Mechanisms, models, and markers. Curr Drug Metab 19, 808-818. doi:10.2174/1389200219666180427165035
Chen, C., Krausz, K. W., Shah, Y. M. et al. (2009). Serum metabolomics reveals irreversible inhibition of fatty acid β-oxidation through the suppression of PPARα activation as a contributing mechanism of acetaminophen-induced hepatotoxicity. Chem Res Toxicol 22, 699-707. doi:10.1021/tx800464q
Choudhuri, S., Patton, G. W., Chanderbhan, R. F. et al. (2018). From classical toxicology to Tox21: Some critical conceptual and technological advances in the molecular understanding of the toxic response beginning from the last quarter of the 20th century. Toxicol Sci 161, 5-22. doi:10.1093/toxsci/kfx186
Dasgupta, A. and Klein, K. (2014). Chapter 2 – Methods for measuring oxidative stress in the laboratory. Antioxidants in Food, Vitamins and Supplements (19-40). Elsevier. doi:10.1016/b978-0-12-405872-9.00002-1
European Union (2006). Regulation (EC) No 1907/2006 of the European Parliament and of the Council of 18 December 2006 concerning the Registration, Evaluation, Authorisation and Restriction of Chemicals (REACH), establishing a European Chemicals Agency, amending Directive 1999/45/EC and repealing Council Regulation (EEC) No 793/93 and Commission Regulation (EC) No 1488/94 as well as Council Directive 76/769/EEC and Commission Directives 91/155/EEC, 93/67/EEC, 93/105/EC and 2000/21/EC. OJ L 396, 1-849.
European Union (2009). Regulation (EC) No 1223/2009 of the European Parliament and of the Council of 30 November 2009 on cosmetic products. OJ L 342, 59-209.
Fan, X., Lobenhofer, E. K., Chen, M. et al. (2010). Consistency of predictive signature genes and classifiers generated using different microarray platforms. Pharmacogenomics 10, 247-257. doi:10.1038/tpj.2010.34
Farmahin, R., Williams, A., Kuo, B. et al. (2017). Recommended approaches in the application of toxicogenomics to derive points of departure for chemical risk assessment. Arch Toxicol 91, 2045-2065. doi:10.1007/s00204-016-1886-5
Farré, M., Roset, P. N., Abanades, S. et al. (2008). Study of paracetamol 1g oral solution bioavailability. Methods Find Exp Clin Pharmacol 30, 37-41. doi:10.1358/mf.2008.30.1.1159648
Friedman, K. P., Gagne, M., Loo, L. H. et al. (2020). Utility of in vitro bioactivity as a lower bound estimate of in vivo adverse effect levels and in risk-based prioritization. Toxicol Sci 173, 202-225. doi:10.1093/toxsci/kfz201
Gijbels, E., Vilas-Boas, V., Deferm, N. et al. (2019). Mechanisms and in vitro models of drug-induced cholestasis. Arch Toxicol 93, 1169-1186. doi:10.1007/s00204-019-02437-2
Gijbels, E., Vilas‐Boas, V., Annaert, P. et al. (2020). Robustness testing and optimization of an adverse outcome pathway on cholestatic liver injury. Arch Toxicol 94, 1151-1172. doi:10.1007/s00204-020-02691-9
Grefhorst, A., van de Peppel, I. P., Larsen, L. E. et al. (2021). The role of lipophagy in the development and treatment of non-alcoholic fatty liver disease. Front Endocrinol 11, 601627. doi:10.3389/fendo.2020.601627
Grünig, D., Szabo, L., Marbet, M. et al. (2020). Valproic acid affects fatty acid and triglyceride metabolism in HepaRG cells exposed to fatty acids by different mechanisms. Biochem Pharmacol 177, 113860. doi:10.1016/j.bcp.2020.113860
Gu, X. and Manautou, J. E. (2012). Molecular mechanisms underlying chemical liver injury. Expert Rev Mol Med 14, e4. doi:10.1017/S1462399411002110
Guillouzo, A., Corlu, A., Aninat, C. et al. (2007). The human hepatoma HepaRG cells: A highly differentiated model for studies of liver metabolism and toxicity of xenobiotics. Chem Biol Interact 168, 66-73. doi:10.1016/j.cbi.2006.12.003
Guo, L., Lobenhofer, E. K., Wang, C. et al. (2006). Rat toxicogenomic study reveals analytical consistency across microarray platforms. Nat Biotechnol 24, 1162-1169. doi:10.1038/nbt1238
Gustafson, E., Debruyne, C., De Troyer, O. et al. (2020). Screening of repeated dose toxicity data in safety evaluation reports of cosmetic ingredients issued by the scientific committee on consumer safety between 2009 and 2019. Arch Toxicol 94, 3723-3735. doi:10.1007/s00204-020-02868-2
Hamon, J., Jennings, P. and Bois, F. Y. (2014). Systems biology modeling of omics data: Effect of cyclosporine a on the Nrf2 pathway in human renal cells. BMC Syst Biol 8, 76. doi:10.1186/1752-0509-8-76
Harrill, J., Shah, I., Setzer, R. W. et al. (2019). Considerations for strategic use of high-throughput transcriptomics chemical screening data in regulatory decisions. Curr Opin Toxicol 15, 64-75. doi:10.1016/j.cotox.2019.05.004
Harrill, J. A., Everett, L. J., Haggard, D. E. et al. (2024). Exploring the effects of experimental parameters and data modeling approaches on in vitro transcriptomic point-of-departure estimates. Toxicology 501, 153694. doi:10.1016/j.tox.2023.153694
Hayes, A. W. and Kruger, C. L. (eds.) (2014). Hayes’ Principles and Methods of Toxicology (6th edition). CRC Press, Taylor and Francis Group. doi:10.1201/b17359
Ipsen, D. H., Lykkesfeldt, J. and Tveden-Nyborg, P. (2018). Molecular mechanisms of hepatic lipid accumulation in non-alcoholic fatty liver disease. Cell Mol Life Sci 75, 3313-3327. doi:10.1007/s00018-018-2860-6
Itabe, H., Yamaguchi, T., Nimura, S. et al. (2017). Perilipins: A diversity of intracellular lipid droplet proteins. Lipids Health Dis 16, 83. doi:10.1186/s12944-017-0473-y
Jaeschke, H., McGill, M. R. and Ramachandran, A. (2012). Oxidant stress, mitochondria, and cell death mechanisms in drug-induced liver injury: Lessons learned from acetaminophen hepatotoxicity. Drug Metab Rev 44, 88-106. doi:10.3109/03602532.2011.602688
Jaeschke, H. and Ramachandran, A. (2018). Oxidant stress and lipid peroxidation in acetaminophen hepatotoxicity. React Oxyg Species (Apex, N.C.) 5, 145-158.
James, L. P., Capparelli, E. V., Simpson, P. M. et al. (2008). Acetaminophen-associated hepatic injury: Evaluation of acetaminophen protein adducts in children and adolescents with acetaminophen overdose. Clin Pharmacol Ther 84, 684-690. doi:10.1038/clpt.2008.190
Johnson, K. J., Auerbach, S. S., Stevens, T. et al. (2022). A transformative vision for an omics-based regulatory chemical testing paradigm. Toxicol Sci 190, 127-132. doi:10.1093/toxsci/kfac097
Kadmon, M., Klünemann, C., Böhme, M. et al. (1993). Inhibition by cyclosporin A of adenosine triphosphate-dependent transport from the hepatocyte into bile. Gastroenterology 104, 1507-1514. doi:10.1016/0016-5085(93)90363-h
Kennedy, D., Samali, A. and Jäger, R. (2015). Methods for studying ER stress and UPR markers in human cells. In C. Oslowski (ed.), Stress Responses (3-18). Methods in Molecular Biology, Volume 1292. New York, NY, USA: Humana Press. doi:10.1007/978-1-4939-2522-3_1
Kralj, T., Brouwer, K. L. R. and Creek, D. J. (2021). Analytical and omics-based advances in the study of drug-induced liver injury. Toxicol Sci 183, 1-13. doi:10.1093/toxsci/kfab069
Kuleshov, M. V., Jones, M. R., Rouillard, A. D. et al. (2016). Enrichr: A comprehensive gene set enrichment analysis web server 2016 update. Nucleic Acids Res 44, W90-W97. doi:10.1093/nar/gkw377
Kültz, D. (2005). Molecular and evolutionary basis of the cellular stress response. Ann Rev Physiol 67, 225-257. doi:10.1146/annurev.physiol.67.040403.103635
Lichtenstein, D., Luckert, C., Alarcan, J. et al. (2020). An adverse outcome pathway-based approach to assess steatotic mixture effects of hepatotoxic pesticides in vitro. Food Chem Toxicol 139, 111283. doi:10.1016/j.fct.2020.111283
Liu, X., Taylor, S. A., Celaj, S. et al. (2022). Expression of unfolded protein response genes in post-transplantation liver biopsies. BMC Gastroenterology 22, 380. doi:10.1186/s12876-022-02459-8
Liu, Z., Huang, R., Roberts, R. et al. (2019). Toxicogenomics: A 2020 vision. Trends Pharmacol Sci 40, 92-103. doi:10.1016/j.tips.2018.12.001
Love, M. I., Huber, W. and Anders, S. (2014). Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol 15, 550. doi:10.1186/s13059-014-0550-8
Luckert, C., Braeuning, A., de Sousa, G. et al. (2018). Adverse outcome pathway-driven analysis of liver steatosis in vitro : A case study with cyproconazole. Chem Res Toxicol 31, 784-798. doi:10.1021/acs.chemrestox.8b00112
Malhotra, J. D. and Kaufman, R. J. (2007). Endoplasmic reticulum stress and oxidative stress: A vicious cycle or a double-edged sword? Antioxid Redox Signal 9, 2277-2294. doi:10.1089/ars.2007.1782
McGill, M. R. and Jaeschke, H. (2013). Metabolism and disposition of acetaminophen: Recent advances in relation to hepatotoxicity and diagnosis. Pharm Res 30, 2174-2187. doi:10.1007/s11095-013-1007-6
Mellor, C. L., Steinmetz, F. P. and Cronin, M. T. D. (2016). The identification of nuclear receptors associated with hepatic steatosis to develop and extend adverse outcome pathways. Crit Rev Toxicol 46, 138-152. doi:10.3109/10408444.2015.1089471
More, S. J., Bampidis, V., Benford, D. et al. (2022). Guidance on the use of the benchmark dose approach in risk assessment. EFSA J 20, e07584. doi:10.2903/j.efsa.2022.7584
National Toxicology Program (2018). NTP Research Report on National Toxicology Program Approach to Genomic Dose-Response Modeling. doi:10.22427/ntp-rr-5
Nguyen, P., Leray, V., Diez, M. et al. (2008). Liver lipid metabolism. J Anim Physiol Anim Nutr 92, 272-283. doi:10.1111/j.1439-0396.2007.00752.x
Pacheco-Alvarez, D., Solórzano-Vargas, R. S. and del Río, A. L. (2002). Biotin in metabolism and its relationship to human disease. Arch Med Res 33, 439-447. doi:10.1016/s0188-4409(02)00399-5
Panico, A., Serio, F., Bagordo, F. et al. (2019). Skin safety and health prevention: An overview of chemicals in cosmetic products. J Prev Med Hyg 60, E50-E57. doi:10.15167/2421-4248/jpmh2019.60.1.1080
Pavlik, L., Regev, A., Ardayfio, P. A. et al. (2019). Drug-induced steatosis and steatohepatitis: The search for novel serum biomarkers among potential biomarkers for non-alcoholic fatty liver disease and non-alcoholic steatohepatitis. Drug Safety 42, 701-711. doi:10.1007/s40264-018-00790-2
Phillips, J. R., Svoboda, D. L., Tandon, A. et al. (2019). BMDExpress 2: Enhanced transcriptomic dose-response analysis workflow. Bioinformatics 35, 1780-1782. doi:10.1093/bioinformatics/bty878
Podtelezhnikov, A. A., Monroe, J. J., Aslamkhan, A. G. et al. (2020). Quantitative transcriptional biomarkers of xenobiotic receptor activation in rat liver for the early assessment of drug safety liabilities. Toxicol Sci 175, 98-112. doi:10.1093/toxsci/kfaa026
Price, R. J., Scott, M. P., Giddings, A. M. et al. (2008). Effect of butylated hydroxytoluene, curcumin, propyl gallate and thiabendazole on cytochrome P450 forms in cultured human hepatocytes. Xenobiotica 38, 574-586. doi:10.1080/00498250802008615
Ramachandran, A. and Jaeschke, H. (2018). Acetaminophen toxicity: Novel insights into mechanisms and future perspectives. Gene Expr 18, 19-30. doi:10.3727/105221617x15084371374138
Ramaiahgari, S. C., Waidyanatha, S., Dixon, D. et al. (2017). From the cover: Three-dimensional (3D) HepaRG spheroid model with physiologically relevant xenobiotic metabolism competence and hepatocyte functionality for liver toxicity screening. Toxicol Sci 159, 124-136. doi:10.1093/toxsci/kfx122
Ramaiahgari, S. C., Auerbach, S. S., Saddler, T. O. et al. (2019). The power of resolution: Contextualized understanding of biological responses to liver injury chemicals using high-throughput transcriptomics and benchmark concentration modeling. Toxicol Sci 169, 553-566. doi:10.1093/toxsci/kfz065
Rao, S. R., Ajitkumar, S., Subbarayan, R. et al. (2018). Cyclosporine-A induces endoplasmic reticulum stress in human gingival fibroblasts – An in vitro study. J Oral Biol Craniofac Res 8, 165-167. doi:10.1016/j.jobcr.2016.11.002
Reardon, A. J. F., Farmahin, R., Williams, A. et al. (2023). From vision toward best practices: Evaluating in vitro transcriptomic points of departure for application in risk assessment using a uniform workflow. Front Toxicol 5, 1194895. doi:10.3389/ftox.2023.1194895
Rogiers, V., Benfenati, E., Bernauer, U. et al. (2020). The way forward for assessing the human health safety of cosmetics in the EU – Workshop proceedings. Toxicology 436, 152421. doi:10.1016/j.tox.2020.152421
Román, I. D. and Coleman, R. (1994). Disruption of canalicular function in isolated rat hepatocyte couplets caused by cyclosporin A. Biochem Pharmacol 48, 2181-2188. doi:10.1016/0006-2952(94)90352-2
Russmann, S., Kullak-Ublick, G. and Grattagliano, I. (2009). Current concepts of mechanisms in drug-induced hepatotoxicity. Curr Med Chem 16, 3041-3053. doi:10.2174/092986709788803097
Saarimäki, L. A., Morikka, J., Pavel, A. et al. (2023). Toxicogenomics data for chemical safety assessment and development of new approach methodologies: An adverse outcome pathway-based approach. Adv Sci (Weinh) 10, e2203984. doi:10.1002/advs.202203984
SCCS (2009). Scientific Committee on Consumer Safety, opinion on Triclosan, addemdum to the SCCP opinion on Triclosan (SCCP/1192/08). doi:10.2772/96027
SCCS (2010). Scientific Committee on Consumer Safety, opinion on 2,7-Naphthalenediol, COLIPA No. A19. doi:10.2772/27368
SCCS (2021a). Scientific Committee on Consumer Safety, opinion on Butylated Hydroxytoluene (BHT). doi:10.2875/53206
SCCS (2021b). The SCCS Notes of Guidance for the Testing of Cosmetic Ingredients and their Safety Evaluation, 11th revision. doi:10.2875/273162
Schumacher, J. and Guo, G. (2015). Mechanistic review of drug-induced steatohepatitis. Toxicol Appl Pharmacol 289, 40-47. doi:10.1016/j.taap.2015.08.022
Selvaraj, S., Oh, J.-H. and Borlak, J. (2020). An adverse outcome pathway for immune-mediated and allergic hepatitis: A case study with the NSAID diclofenac. Arch Toxicol 94, 2733-2748. doi:10.1007/s00204-020-02767-6
Sevilla-Tirado, F. J., Gonzalez-Vallejo, E. B., Leary, A. C. et al. (2003). Bioavailability of two new formulations of paracetamol, compared with three marketed formulations, in healthy volunteers. Methods Find Exp Clin Pharmacol 25, 531-535. doi:10.1358/mf.2003.25.7.778092
Sharanek, A., Azzi, P. B.-E., Al-Attrache, H. et al. (2014). Different dose-dependent mechanisms are involved in early cyclosporine A-induced cholestatic effects in HepaRG cells. Toxicol Sci 141, 244-253. doi:10.1093/toxsci/kfu122
Sharanek, A., Burban, A., Humbert, L. et al. (2015). Cellular accumulation and toxic effects of bile acids in cyclosporine A-treated HepaRG hepatocytes. Toxicol Sci 147, 573-587. doi:10.1093/toxsci/kfv155
Song, Y., Zhang, C., Lei, H. et al. (2022). Characterization of triclosan-induced hepatotoxicity and triclocarban-triggered enterotoxicity in mice by multiple omics screening. Sci Total Environ 838, 156570. doi:10.1016/j.scitotenv.2022.156570
Spyker, D. A., Dart, R. C., Yip, L. et al. (2022). Population pharmacokinetic analysis of acetaminophen overdose with immediate release, extended release and modified release formulations. Clin Toxicol 60, 1113-1121. doi:10.1080/15563650.2022.2114361
Sutherland, J. J., Jolly, R. A., Goldstein, K. M. et al. (2016). Assessing concordance of drug-induced transcriptional response in rodent liver and cultured hepatocytes. PLoS Comput Biol 12, e1004847. doi:10.1371/journal.pcbi.1004847
Sutherland, J. J., Webster, Y. W., Willy, J. A. et al. (2018). Toxicogenomic module associations with pathogenesis: A network-based approach to understanding drug toxicity. Pharmacogenomics J 18, 377-390. doi:10.1038/tpj.2017.17
Sztalryd, C. and Kimmel, A. R. (2014). Perilipins: Lipid droplet coat proteins adapted for tissue-specific energy storage and utilization, and lipid cytoprotection. Biochimie 96, 96-101. doi:10.1016/j.biochi.2013.08.026
Tan, C. and Graudins, A. (2006). Comparative pharmacokinetics of panadol extend and immediate-release paracetamol in a simulated overdose model. Emerg Med Australas 18, 398-403. doi:10.1111/j.1742-6723.2006.00873.x
Tanabe, S., O’Brien, J., Tollefsen, K. E. et al. (2022). Reactive oxygen species in the adverse outcome pathway framework: Toward creation of harmonized consensus key events. Front Toxicol 4, 887135. doi:10.3389/ftox.2022.887135
Tazuma, S. (2006). Cyclosporin A and cholestasis: Its mechanism(s) and clinical relevancy. Hepatol Res 34, 135-136. doi:10.1016/j.hepres.2005.12.009
Thomas, R. S., Philbert, M. A., Auerbach, S. S. et al. (2013a). Incorporating new technologies into toxicity testing and risk assessment: Moving from 21st century vision to a data-driven framework. Toxicol Sci 136, 4-18. doi:10.1093/toxsci/kft178
Thomas, R. S., Wesselkamper, S. C., Wang, N. C. Y. et al. (2013b). Temporal concordance between apical and transcriptional points of departure for chemical risk assessment. Toxicol Sci 134, 180-194. doi:10.1093/toxsci/kft094
Thomas, R. S., Bahadori, T., Buckley, T. J. et al. (2019). The next generation blueprint of computational toxicology at the U.S. environmental protection agency. Toxicol Sci 169, 317-332. doi:10.1093/toxsci/kfz058
Vahle, J. L., Anderson, U., Blomme, E. A. G. et al. (2018). Use of toxicogenomics in drug safety evaluation: Current status and an industry perspective. Regul Toxicol Pharmacol 96, 18-29. doi:10.1016/j.yrtph.2018.04.011
van Breda, S. G. J., Claessen, S. M. H., van Herwijnen, M. et al. (2018). Integrative omics data analyses of repeated dose toxicity of valproic acid in vitro reveal new mechanisms of steatosis induction. Toxicology 393, 160-170. doi:10.1016/j.tox.2017.11.013
Van den Hof, W. F. P. M., Ruiz-Aracama, A., Van Summeren, A. et al. (2015). Integrating multiple omics to unravel mechanisms of cyclosporin A induced hepatotoxicity in vitro. Toxicol In Vitro 29, 489-501. doi:10.1016/j.tiv.2014.12.016
Verheijen, M. CT., Meier, M. J., Asensio, J. O. et al. (2022). R-ODAF: Omics data analysis framework for regulatory application. Regul Toxicol Pharmacol 131, 105143. doi:10.1016/j.yrtph.2022.105143
Vinken, M., Pauwels, M., Ates, G. et al. (2012). Screening of repeated dose toxicity data present in SCC(NF)P/SCCS safety evaluations of cosmetic ingredients. Arch Toxicol 86, 405-412. doi:10.1007/s00204-011-0769-z
Vinken, M., Landesmann, B., Goumenou, M. et al. (2013a). Development of an adverse outcome pathway from drug-mediated bile salt export pump inhibition to cholestatic liver injury. Toxicol Sci 136, 97-106. doi:10.1093/toxsci/kft177
Vinken, M., Maes, M., Vanhaecke, T. and Rogiers, V. (2013b). Drug-induced liver injury: Mechanisms, types and biomarkers. Curr Med Chemi 20, 3011-3021. doi:10.2174/0929867311320240006
Vinken, M. (2019). Omics-based input and output in the development and use of adverse outcome pathways. Curr Opin Toxicol 18, 8-12. doi:10.1016/j.cotox.2019.02.006
Vitale, G., Mattiaccio, A., Conti, A. et al. (2023). Molecular and clinical links between drug-induced cholestasis and familial intrahepatic cholestasis. Int J Mol Sci 24, 5823. doi:10.3390/ijms24065823
Vrijenhoek, N., Wehr, M. M., Kunnen, S. J. et al. (2022). Application of high-throughput transcriptomics for mechanism-based biological read-across of short-chain carboxylic acid analogues of valproic acid. ALTEX 39, 207-220. doi:10.14573/altex.2107261
Wang, C., Gong, B., Bushel, P. R. et al. (2014). The concordance between RNA-seq and microarray data depends on chemical treatment and transcript abundance. Nat Biotechnol 32, 926-932. doi:10.1038/nbt.3001
Xie, Y., McGill, M. R., Cook, S. F. et al. (2015). Time course of acetaminophen-protein adducts and acetaminophen metabolites in circulation of overdose patients and in HepaRG cells. Xenobiotica 45, 1574-1583. doi:10.3109/00498254.2015.1026426
Xu, S., Chen, Y., Ma, Y. et al. (2019). Lipidomic profiling reveals disruption of lipid metabolism in valproic acid-induced hepatotoxicity. Front Pharmacol 10, 819. doi:10.3389/fphar.2019.00819
Yasumiba, S., Tazuma, S., Ochi, H. et al. (2001). Cyclosporin A reduces canalicular membrane fluidity and regulates transporter function in rats. Biochem J 354, 591-596. doi:10.1042/0264-6021:3540591
Yeakley, J. M., Shepard, P. J., Goyena, D. E. et al. (2017). A trichostatin A expression signature identified by TempO-Seq targeted whole transcriptome profiling. PLoS One 12, e0178302. doi:10.1371/journal.pone.0178302
Yin, W., Mendoza, L., Monzon-Sandoval, J. et al. (2021). Emergence of co-expression in gene regulatory networks. PLoS One 16, e0247671. doi:10.1371/journal.pone.0247671
Yoon, E., Babar, A., Choudhary, M. et al. (2016). Acetaminophen-induced hepatotoxicity: A comprehensive update. J Clin Transl Hepatol 4, 131-142. doi:10.14218/jcth.2015.00052
Zoupa, M., Zwart, E. P., Gremmer, E. R. et al. (2020). Dose addition in chemical mixtures inducing craniofacial malformations in zebrafish (Danio rerio) embryos. Food Chem Toxicol 137, 111117. doi:10.1016/j.fct.2020.111117